Juniper Publishers: Atypical Presentation of Invasive Mole in a Young Female with Chemo resistance Case Report and Review of Literature
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Rajshree Dayanand Katke*
Abstract
Gestational trophoblastic neoplasias (GTN) are rare
tumours that constitute less than 1% of all gynecological malignancies.
Invasive mole is a condition where a molar pregnancy, such as a partial
hydatidiform mole or complete hydatidiform mole, invades the wall of the
uterus, potentially spreading and metastasizing to other parts of the
body. Invasive mole is a distinct subgroup of GTN, which if not
diagnosed and treated early, can result in serious complications like
uterine perforation and haemoperitoneum. We present a rare case of
anchemoresistant invasive mole of the uterus, which developed following
the evacuation of a molar pregnancy. It was accurately diagnosed and
successfully treated before any major complications could arise.
Keywords: Complete hydatiform mole; Invasive mole; Beta-human chorionic gonadotropin; Haemoperitoneum; ChemoresistantIntroduction
Gestational Trophoblastic Disease (GTD) is an
umbrella term for a group of pregnancy related disorders arising from
abnormal placental trophoblast cells. It encompasses two pre-malignant
conditions: partial and complete hydatidiform moles and the malignant
Gestational Trophoblastic Neoplasias (GTN). GTNs are classified
histologically into three distinct subgroups: choriocarcinomadestruens
(invasive mole), choriocarcinoma (CC) and the very rare placental site
trophoblastic tumor (PSTT) [1].
Invasive moles are responsible for most cases of localized GTN.
Invasive moles have high potential of metastasizing and local invasion
causing hemoperitoneum Invasive mole is condition where a molar
pregnancy invades the wall of the uterus. It follows approximately 10-
15% of complete hydatidiform moles and 0.5% of patients with partial
mole [2].
For Invasive mole the imaging of choice is B-mode ultrasonography and
color Doppler. When ultrasonography corresponds with the classical
clinical presentation, an accurate diagnosis is possible in a majority
of cases. With early and accurate diagnosis, the cure rate is high.
Treatment of an invasive mole may include both chemotherapy and surgery.
Case Report
28 years old Female, gravida three para one living
one abortion one with previous ceasearian section came to our OPD with
the chief complaints of two months of amenorrhea with bleeding per
vaginum since one day and with ultrasonography report suggestive of
vesicular mole. By last menstrual period patient has 9 weeks of
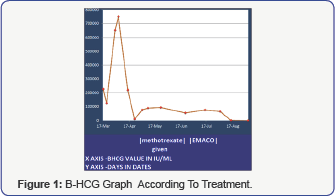
gestation. On general examination patient was vitally stable (Figure 1-3).
On per abdominal examination abdomen was soft and
patient was obese there was no guarding tenderness or rigidity. On per
speculum spotting was present and on per vaginum uterus was 12-14 weeks
size and cervical os was closed. Patient all routine, serum beta human
chorionic gonadotropin, ecg, xray, thyroid function test was done
immediately. Her Serum beta human chorionic gonadotropine (beta hCG) was
225000 IU. Her all routine and thyroid function test was within normal
limits. Chest x-ray was normal. Patient was taken for suction
evacuation. Repeat B-hcg was done on day 3 post suction evacuation was
125000 IU/ML. Patient took discharge and again follow up after one week
with complaint of spotting per vaginum and fresh beta-hcg report with
value of 750000 IU. We have done urgent ultrasound of the patient which
was suggestive of hyadatiform mole? invasion asendomyometrial junction
is not well demarcated. We started patient on single agent chemotherapy.
After one cycle serum beta hcg was repeated and was 225000 iu /ml.
Repeat ultrasound was done suggestive of decrease in size of uterus
since previous scan residual lesion is still significant with well
defined endimyometrial junction. Hence decision of repeat suction
evacuation was done.
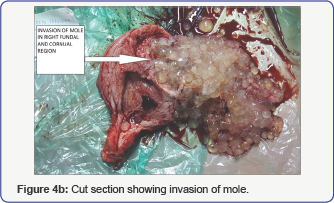
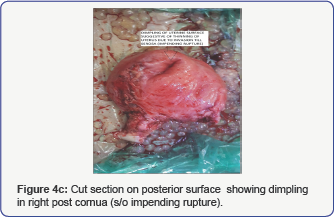
Repeat serum beta-hcg was less than 10000 iu/ml. But
still for safer practice we have done repeat ultrasound for the patient
which shows residual mole invading the myometrium and repeat serum beta
hcg also raised to 75000 from 10000 iu. Patient was started on EMACO
REGIMEN. three cycle of EMACO regimen was given. HRCT SCAN was done and
was normal. Patient’s serum beta hcg was repeated and there was no
significant change in the beta hcg values. MRI was done and was
suggestive of multicystic lesion of size 8.7x6.3x7 cm septate involving
myometrium s/o invasive mole with no extrauterine spread and no
lymphadenopathy. There was no significant decrease in size of lesion and
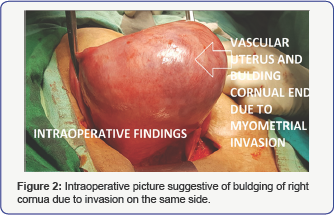
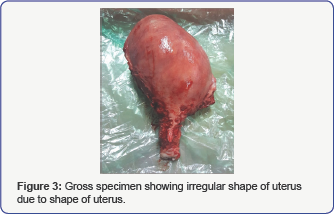
serum b hcg level even after three cycles of EMACO regimen. Hence tough
decision hysterectomy was done in view of chemoresistant invasive
persistent trophoblastic disease. Her post operative period was
uneventful.post operative value of serum betahcg was 165 iu/ml. patient
was discharge on post operative day 7. Patient last follow up serum bhcg
was 4 iu/ml.
Discussion
Gestational trophoblastic neoplasia, 60% was
secondary to hydatidiform mole, 30% to abortion, and 10% secondary to
full term pregnancy or ectopic pregnancy. According to the
epidemiological retrospective survey, invasive mole was diagnosed as
secondary to hydatidi form mole emptying within half a year and
choriocarcinoma was mostly more than a year. Clinical manifestations of
GTN involve full-term vaginal bleeding after childbirth, ectopic
pregnancy and (or) corresponding signs and symptoms of metastatic organs
[3].
CT, MRI, biopsy, blood HCG test, cystoscope, and
laparoscopic examination are typically used as evaluation means and
methods. Histological diagnosis is the gold standard, but sometimes we
can only based on clinical diagnosis without histological evidence.
Gestational trophoblastic tumor is typically sensitive to chemotherapy,
and the cure rate about 80% to 90%. International Federation of
Gynecologists and Obstetricians (FIGO) found prognostic scoring system
in which gestational trophoblastic tumors are divided into low-risk and
high-risk groups [4].
Patients in low-risk group, generally are carried
with single-agent chemotherapy such as Methotrexate (MTX) or actinomycin
D treatment, while the high-risk group with multi-drug chemotherapy
regimens, and EMA-CO is commonly used chemotherapy regimens [5].
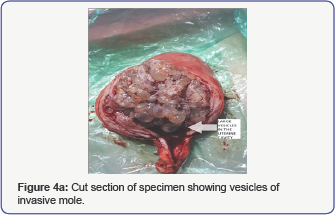
As in our case the diseases progresses very rapidly and was almost
progressed uptoserosa, hence increases chances of metastasis,
perforation, acute hemoperitoneum etc. Preoperative X-ray chest
hemogram, baseline B-HCG, blood grouping, liver enzymes done routinely
before suction Evacuation (Figure 4a-4c).
It is also an important adjunct to the treatment of
chemo-resistant tumors. Chemotherapy is now the established method of
treatment of choriocarcinoma and hysterectomy and surgical resection of
the tumor is rarely required in cases resistant to chemotherapy [6].
In summary, GTN as a curable tumor, even if resistance, and its general
principle of treatment is to cure and not just to prolong survival
time. To patients at high risk and chemoresistance, we should emphasize
the extent of disease and the previous treatments, to develop
individualized treatment programs. In addition, we should also emphasize
the important of surgical treatment, take a comprehensive assessment of
the patient’s condition, apply chemotherapy actively, fight for
surgical resection resistant lesions, in order to achieve the ultimate
goal of sustained remission. Continuous monitoring blood HCG levels [7] and imaging examination [8], both of which are available methods to determine GTN therapeutic effect and recurrence.
Conclusion
Our case report emphasizes that persistent
trophoblastic disease needs to be defined precisely and early diagnosis
and treatment. Chemoresistant invasive mole surgical intervention at
proper time in management of persistent trophoblastic disease is the key
to 100% survival in gestational trophoblastic neoplasia. Furthermore,
early diagnosis by ultrasound and histopathological examination is the
key to avoid associated complications such as acute hemoperitoneum,
perforation metastasis, hyperemesis gravidarum, hyperthyroidism, and
preeclampsia. Our case also proves that there is complete remission with
no metastasis of chemoresistent invasive mole if early diagnosis and
correct decision of appropriate treatment is done.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment