Juniper Publishers: A Case Report and Review of the Literature
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Rosario Fernandez Salmerón
Abstract
Background: Dermatomyositis (DM)
is a rare paraneoplasic neurological syndrome (PNS) that may precedes
the development of malignancies. It´s an uncommon inflammatory myophaty
with characteristic cutaneous manifestations. The association between DM
and cancer has long been recognized but is becoming more clearly
delineated. Several studies have documented an increased rate of
malignant disease associated with DM over that observed in the general
population. The incidence of ovarian cancer developing in the setting of
DM was reported to be as high as 13.3 % in one series.
Case report: We report a
case of a 50 years old postmenopausal woman who developed a progressive
muscle weakness abd cutaneous rash that was finally diagnosed as DM. On
CT abdomen explorataion a complex right adnexal mass was described. CA
-125 was elevated. Exploratory laparotomy found a nonadherent enlarged
right ovary with no surface excrescences or peritoneal spread.
Histologically was high-grade serous papillary adenocarcinoma.
Conclusion: Screening for tumours is important in patients with a previous diagnosis of DM or other PNS.
Introduction
DM is an inflammatory myopathy with well-defined
pathological features including the microangiopathy. DM is frecuently
associated with concomitant cancers, as many as 25% of cases are
associated with an occult neoplasm [1]. This paraneoplastic syndrome may
precede the development of malignancies such as lung, breast, or
ovarian cancer by several months and even years [2]. It is a rare
inflammatory myopathy with characteristic cutaneous manifestations.
Criteria for this disease are progressive, proximal and symetrical
weakness, and increased concentrationof muscle enzymes, an abnormal
electromyogram, an abnormal muscle biopsy sample, and compatible
cutaneous disease [3]. A rash that occurs in a shawl-like distribution
is characteristic of this disease, as is proximal muscle weakness and
elevation of serum creatine kinase levels. The cutaneous manifestations
include heliotrope rash, cuticular changes, a photo distributed
erythema, and a scaly alopecia. The pathogenesis of the skin lesions or
dermatomyositis is not understood.
The association between DM and cancer has long been
recognized but is becoming more clearly delineated. Several Scandinavian
studies have documented an increased rate of malignatn disease
associated with DM over the observed in the general population [4,5].
The incidence of ovarian cancer developing in the setting of DM was
reported to be as high as 13.3 % in one series [2].
Screening for tumours is important in patients with a
previous diagnosis of DM or other PNS as the early diagnosis of the
tumour directly affects prognosis [6]. Because of the rare correlation
between ovarian carcinoma and the DM, we present our case and review the
literature-
Case

50 years-old white woman, who was 4 years postmenopausal
was referred to the emergency department with muscle weakness
in arms and legs. Furthermore, she had a pruritic skin rush for
three months believed to be secondary tu sun exposure. Physical
examination found cutaneous lesions that were erythematous,
slightly scaly, macular and papular, involving the neck, upper
chest, front, back, arms and hands (Figure 1).
There was violaceous facial erythema with a heliotrope
eyelid rash and deep violaceous color on the extensor surfaces
of fer fingers, elbows and knees. She had loss of proximal
muscle strength. The medical history included bipolar
disorder, appendicectomy and carpal tunnel syndrome surgery.
Mammogram was normal and her previous Papanicolaou smear
and pelvic examination were normal 2 years before admission.
Laboratory findings included creatinine phosphokinase of
3572 U/mL (normal 0-170), deshidrogenase lactate of 1006
(normal 230-460) and light elevation of others liver enzymes,
aldolase of 25 U/Ml (normal 1.8), and a sedimentation rate of 67.
Electromyelogram showed myophatic motor unit potentation
and increased insertional activity consistent with inflammatory
myophaty. CA 125 was 220.1 U/mL (normal 0-35), CA 15.3 was
48.67 (normal 0-25). CEA, alfafetoprotein and CA 19.9 were
normal.
Following Good practice points given (6) her internist
requested a CT-thorax/abdomen, US of the pelvic region and
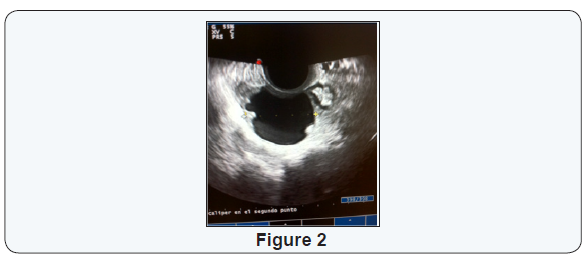
mammography. Trasvaginal ultrasound revealed a 4 cm complex
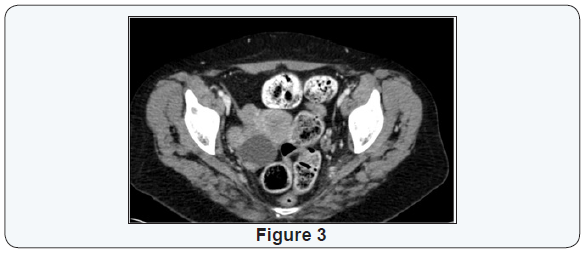
right adnexal cyst with echogenic areas (Figure 2). On CT
abdomen exploration a 4,4 x3,8 cm, complex right adnexal mass
was describes withour ascytis or lymphadenopathy (Figure 3).
Exploratory laparotomy found a nonaherent enlarged right
ovary with no surface excrescences or peritoneal spread. Her
uterous, left ovary, anf fallopian tubes were normal. Intraoperative
biopsy reveled adenocarcinoma. We did a hysterectomy and
billateral salpingo-oophorectomy, omentectomy, and excision of lymph nodes from the common iliac and para-aortic regions.
As well as peritoneal cytologi and apracolic biopsias were
performed.
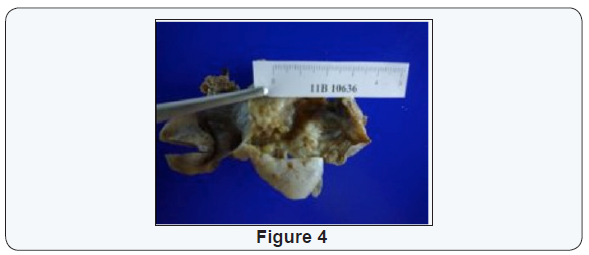
Grossly, the right ovarian neoplasm was a fluid-filled, cystic
tumor measuring 6.5 cm with two solid protuberant masses of
3.5 and 2.5 cm respectively and papillary projections of 5 mm
each one. The capsule was infiltrated. Definitive histopathologic
examination accorging to the International Federation of
Gynecology and Obstetrics (FIGO) revealed a serious papillary
adenocarcinoma, stage IC ovarian carcinoma (Figure 4). The
excised of para-aortic and common iliac lymph nodes showed no
metastasis. Peritoneal cytology and paracolic biopsias were also
negative.
Postoperatively, she received five courses of chemotherapy
with paclitaxel a carboplatin. Her skin condition and muscle
weakness improved soon after the second course of chemotherapy,
approximately 2 months later. The methylprednisolone dose was
tapered until discontinued. Currently the patient is still alive for
2.5 years, without evidence of recurrent disease, since pelvic
examination and transvaginal ultrasonography, as well as CT and
biomarkers (Ca 125: 12 U/mL) are all normal.
Discussion
Despite evidence that ovarian cancer is the most common
gynecologic malignancy in women with dermatomyositis,
the association between the two is rarely appreciated by
ginecologists [2,7-9]. To emphasize the significance of the
coexisting disorders, an ovarian carcinoma presenting initially
as dermatomyositis is described.
The first description of an existing relationship between
malignant disease and myositis was done in 1916 [10]. Since
then, several authors confirmed the association between
malignancy and idiophatic inflammatory myopathies with a
frequency ranging 6-40% [4,11-14]. However clinical outcomes
of the studies are limited by referral bias, lack of controls and
inclusion criteria for myositis.
Polymiositis and dermatomyositis are idiophatic
inflammatory myophaties of undetermined etiology. Connective
tissue diseases present with similar clinical symptoms and
signs like the myopathies and are usually classified together.
Diagnostic criteria por the PM and DM was first suggested by
Bohan and Peter [3].
Two Scandinavian reports (Sweden & Finland) in a
population-based study with PM and DM showed an overall
incidence of associated malignancy 13% and 13.8% respectively
[4,13]. The mean age of patients with myositis relationed with
malignancy is 53 years, ranged from 40 to 66 years [8]. The
association between dermatomyositis and malignant disease is
better established than that of polymyositis. Usually the onset of
dermatomyositis-polimyositis precedes evidence of carcinoma,
ramking from 3 months to 6 years with a mean of 2 years [14],
but it may also present simultaneous with this malignancy
[2,4,15]. In contrast, the development of dermatomyositis after
established diagnosis of ovarian cancer seems to be less common.
The present case report refers to patients with a serious
papillary ovarian adenocarcinoma on a previously established
diagnosis of DM. Our patient demostrates that dermatomyositis
may develop in the setting of pre-existent ovarian cancer and
that skin manifestations may precede clinically obvious, muscle
symptoms by several months. Such patients may experience
improvement in muscle strength with corticosteroid therapy,
despite persistance of skin rash and progression of their
underlying neoplasm.
An autoantibody was recently described in adult patients with
dermatomyositis that seems to be associated with cancer in this
population: the specific antibody transcriptional intermediary
factor 1 gamma (TIF- gamma, initially described as antibody
anti –p155/140) This antibody currently represents the best
marker of neoplasia in dermatomyositis . The antibody positivity
indicates high risk of neoplasia and forces the clinician to closely
monitor the patient with exhaustive screening periodically,
mainly during the first 3 years [16].
The reported frequency of malignancy in dermatomyositis
varies from 6% to 60%, but large population-based cohort
studies report a frequency of 20-25% [17]. Several cancer types
show this association with dermatomyositis. The most common
are ovarian, lung, pancreatic, stomach and colorectalcancers
and lymphomas [18]. The risk for lymphoma was only raised
the first year after diagnosis of dermatomyositis. For the others
tumours, the risk is the highest within the first year of followup
dropping substantially thereafter. The risk for ovarian,
pancreatic and lung cancer remains above average even after 5
years [18]. At diagnosis, thorough examination is requested. In
children, specific attention should be paid to splenomegaly or
lymphadenopathy [19]. In adults, abnormalities should guide
screening tactics, but lack of abnormalities does not imply no
screening is needed. Although the risk rises with age, all adults’
patients should be screened. Women should be screened by US
of the pelvic region and CA-125 and mammography and by CTthorax/
abdomen. Men should be tested by CT- thorax/abdomen.
Men under the age of 50 years should have a US of the testes.
All patients over 50 years old (men and women) should have a
colonoscopy). Screening is to be repeated annually for 3 years.
Afterwards, screening is only performed if new symptoms or finding alerts to it [17-20]. Evidence regarding any additional
value of FDG-PET is lacking.
In conclusion, the detection of ovarian cancer at an early
stage is crucial for patient survival. The physician must be alert
of the possibility of malignancy in patients with a previous
diagnosis of myositis, especially of ovarian carcinoma in the
female population. The current NCCN Clinical Practice Guidelines
in Oncology recommend TV US, combined with cancer antigen
125 (CA-125) each 6 months in patients with genetic/familiar
high risks for ovarian carcinoma [21].
However, screening of such carcinoma including pelvic
examination, transvaginal ultrasonography and CA-125, is not
always effecitve [22]. Because the risk for ovarian, pancreatic
and lung cancer remains above Average even after 5 years [18],
screening is to be repeated annually for 3 years. Afterwards,
screening is only performed if new symptoms or finding alert to
it [17, 20].
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on:https://juniperpublishers.com/jgwh/




Comments
Post a Comment