Juniper Publishers: Comparison of Unidirectional Barbed Suture Compared to Conventional Braided Suture at the Time of Cesarean Section
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Synopsis: Unidirectional barbed suture is not inferior to conventional braided suture at the time of cesarean closure with respect to operative time, blood loss or complications.
Abbreviations: UBS: Unidirectional Braided Suture; CBS: Conventional Braided Suture; BMI: Body Mass Index; EBL: Estimated Blood Loss
To read more......Fulltext in Gynecology
and Women’s Health in Juniper Publishers
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Steven R Lindheim*
Abstract
Background: The bidirectional barbed
suture has been reported as effective as conventional suture in various
soft-tissue closure sites. The objective of this manuscript is to
evaluate peri- and post-operative outcomes using a Unidirectional Barbed
Suture (UBS) compared to Conventional Braided Suture (CBS) at time of
Cesarean section closure.
Methods: This retrospective study
evaluated women (n=138) undergoing cesarean delivery with either UBS
using the V-LocTM wound closure device (Covidien) (n=106) or CBS
(Vicryl®, Ethicon) (n=32) by a single practice. Outcomes measured
included operative time; estimated (EBL) and objective blood loss;
hospital stay; and peri-, postoperative, and overall complications.
Deliveries prior to 28 weeks gestational age and women <18 years of
age were excluded. Student’s t-test and chi-square were used for data
analysis. A p-value <0.05 was considered significant.
Results: Operative time for the UBS
group was similar to the CBS group (35.0 min vs. 35.91 min; p=0.69), as
was EBL (572 mL vs 625 mL, p=0.51); change in hemoglobin (1.8 g/dL vs
1.7 g/dL, p=0.84); hospital stay (3.25d vs 3.19d, p=0.63); and overall
complications (19.8%, n=21 vs 12%, n=4, p=0.35).
Conclusion: UBS is not inferior to
CBS at the time of Cesarean section closure with respect to operative
time, blood loss, or complications, and may be considered as an
adjunctive suture in the closure of the Cesarean incision given the
equal safety and efficacy.
Keywords: Barbed suture; Hysterotomy; Cesarean section; V-LocTMSynopsis: Unidirectional barbed suture is not inferior to conventional braided suture at the time of cesarean closure with respect to operative time, blood loss or complications.
Abbreviations: UBS: Unidirectional Braided Suture; CBS: Conventional Braided Suture; BMI: Body Mass Index; EBL: Estimated Blood Loss
Background
The Quill bidirectional barbed suture was approved by
the United States Food and Drug Administration for soft tissue
approximation in 2004. Since then, there has been reported use of this
and other barbed sutures during surgical and gynecologic procedures.
Recent studies have found the barbed suture is an effective method of
soft tissue closure with non-inferior results to conventional closure
methods with respect to gynecologic procedures. This has been
demonstrated in the setting of closure of the hysterotomy site during
laparoscopic myomectomies [1], closure of the vaginal cuff in laparoscopic hysterectomies [2] and closure of skin incisions during Cesarean section [3] with respect to operative times, estimated blood loss, length of hospital stay and perioperative complications [1-3].
Except for limited study of its use in bovine Cesarean sections [4],
there have been no studies to evaluate the safety, peri-operative
outcomes and efficacy of the barbed suture for closure of the
hysterotomy, peritoneal, fascial incision, subcutaneous tissue and skin
at the time of Cesarean section on human subjects. Thus, the purpose of
this study was to assess outcomes related to the use of Unidirectional
Barbed Suture (UBS) with respect to safety and efficacy compared to
Conventional Braided Suture (CBS) at the time of Cesarean section.
Methods
This retrospective study was reviewed and approved by
the Wright State University, Miami Valley Hospital and United States
Air Force Institutional Review Boards and was in compliance with the
privacy-act guidelines. Informed consent was not required for this
study.
This was a retrospective cohort study of 135 patients
who underwent Cesarean section from January 2008-October 2013 by a
single practitioner at Miami Valley Hospital in Dayton, Ohio. Patients
who underwent Cesarean section with a Pfannenstiel skin incision using
UBS were compared with the patients who underwent Cesarean section with
closure using CBS. Given a single practice, the surgeon primarily used
the V-loc suture and therefore less control subjects were studied in the
given time frame.
Patients under the age of 18 were excluded due to
local IRB requirements and those undergoing delivery at less than 28
weeks gestational age were excluded from the analysis, presumably
because these patients underwent a classical incision during the
Cesarean delivery.
All procedures were performed in the same standard
fashion using a Pfannensteil incision. All hysterotomies were performed
in a transverse fashion through the lower uterine segment. After
delivery of the infant, the placenta was allowed to deliver with gentle
cord traction, and the uterus was exteriorized. For the CBS group, the
hysterotomy was repaired within a single layer with 0-Vicryl® (Ethicon)
in a running locked fashion. Additional suture was used at the surgeon’s
discretion to imbricate the initial closure or to achieve hemostasis.
The peritoneum was closed with 2-0 Vicryl® at the discretion of the
surgeon and the fascia was then closed with 0- Vicryl®.
The subcutaneous tissue was closed with 3-0 Vicryl®
suture at the discretion of the surgeon and the skin was closed with
either conventional suture or staples. The UBS group was closed
similarly with 2-0 V-LocTM (Covidien) for all four layers (hysterotomy;
peritoneum, fascia, subcutaneous layer, and skin). All procedures were
performed by a single surgeon (KW) or supervised by this surgeon.
Patients were typically discharged home on the third postoperative day
and seen as an outpatient within 6 weeks postpartum.
The primary objective was to determine if the UBS had
a non-inferior safety profile compared to CBS with respect to overall
surgical complications. Secondary outcomes measured were operative time,
both total and specifically from hysterotomy closure to skin closure;
blood loss, both subjectively and objectively; as well as length of
hospital stay.
Statistical analyses were performed using the
Statistical Package for the Social Sciences (SPSS version 20.0.0, 2013;
SPSS, Inc., Chicago, IL). Data were expressed as mean ± SD. Unpaired
student test was used to test the significance of differences in means
between groups. Chi-square-test was used to assess the significance of
categorical comparisons. Significance was assessed at p <0.05. Means
were expressed as ± SEM. Statistical analysis was conducted on all
outcomes and between groups.
The data were evaluated for the perioperative
outcomes under study, which were complications, blood loss, duration of
surgery and length of hospital stay. Data was analyzed using a Fisher
exact test and X2 test for all categorical
variables and the t test for continuous variables. All p- values were 2-
sided and p <0.05 was considered statistically significant.
Results
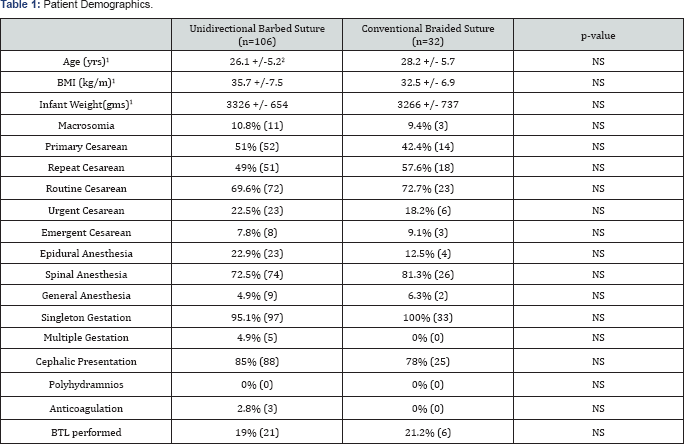
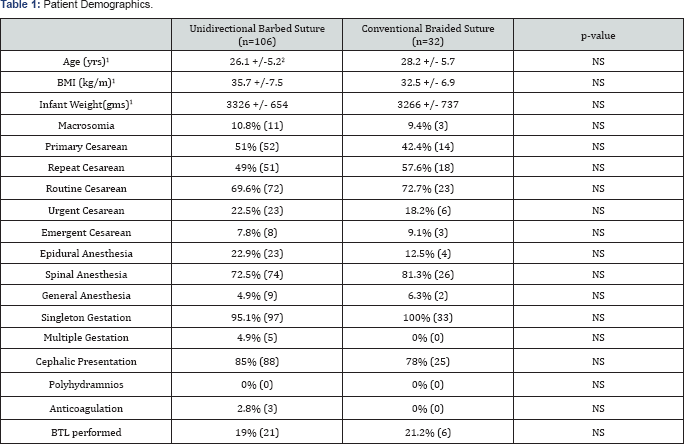
1Mean
2+/- Standard Deviation
There were 142 patients that underwent Cesarean
section in the specified time period. Fourpatients met exclusion
criteria. Patient demographic data are given in (Table 1).
There were no differences between the UBS (n=106) and CBS (n=32) groups
with respect to patient age (26.1 +/-5.2 vs 28.2 +/- 5.7, p-NS) and BMI
(35.7 +/-7.5 vs 32.5 +/- 6.9, p-NS) nor were there differences in the
number of repeat Cesarean sections (49% vs 57.6%,, p-NS), or the number
that underwent general anesthesia (4.9% vs 6.3%, p-NS), multiple
gestation, or on anticoagulation. Those undergoing tubal ligation at the
time of surgery was similar between groups (19% vs 21.2%, p-NS).
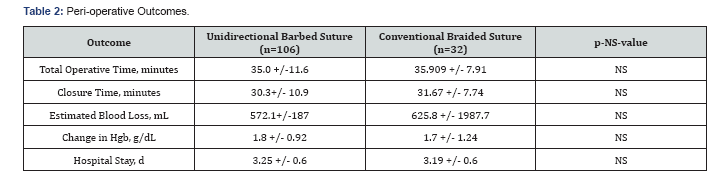
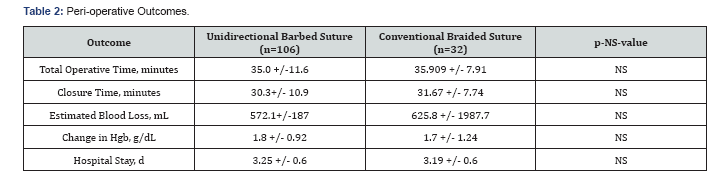
Peri-operative outcomes between the UBS and the CBS groups are given in Table 2.
There were no significant differences in the total operative times
(UBS-35.0 minutes vs. CBS-35.91 minutes, p-NS); closure times (30.2
minutes vs. 31.67 minutes, p-NS); estimated blood loss (572 mL vs 626
mL, p-NS) or decrease in hemoglobin (1.8 g/dL vs 1.7 g/dL, p-NS); or
length of hospital stay (3.25d vs 3.19d, p-NS) (Table 2).
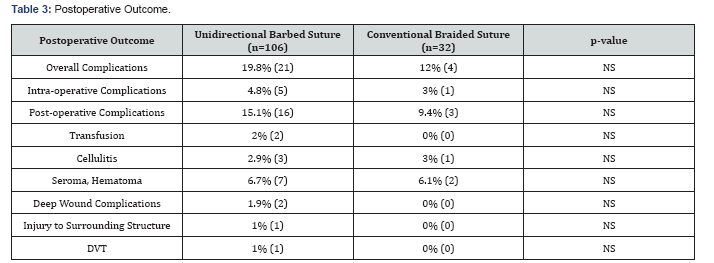
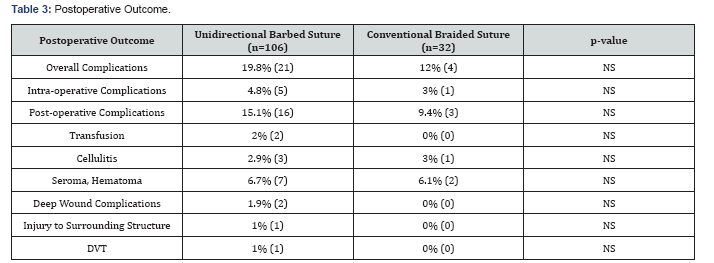
Overall complication rates were similar between the
UBS and CBS groups (19.8%, n=21 vs 12%, n=4, p-NS). Intraoperative
complications were similar between groups (4.8%, n=5 vs 3.0%, n=1, p-NS)
and included two cases of uterine atony (neither requiring a blood
transfusion), one case of uterine rupture identified at the time of
surgery, and three vacuum assistance in delivery of the infant in the
UBS group and one vacuum assistance for delivery in the CBS group.
Post-operative complications were also similar between UBS and CBS
groups: Transfusions (2.0%, n=2 vs 0%, n=0, p-NS); one after planned
Cesarean hysterectomy for known placenta accreta who required a blood
transfusion on postoperative day 2 and the other for symptomatic
postoperative anemia; superficial wound complications (9.4%, n=10vs.
9.4%, n=3, p-NS) which were drained and/or treated with antibiotics,
except for one wound infection which required operative drainage in the
UBS group; and endomyometritis, (1.9%n=2 vs 0%, n=0, p-NS). In the UBS
group, one patient had a suspected nerve entrapment as an injury to a
surrounding structure, but was lost to follow-up. One patient developed a
late pulmonary embolus on postoperative day 22 in the UBS group and was
treated with anticoagulant therapy (Table 3).
Discussion
Our data demonstrates that the UBS is not inferior to
the use of CBS during Cesarean section closure with respect to
operative and post-operative complications and operative time, blood
loss and length of hospital stay.
Since its introduction, there have been few studies addressing the use of barbed suture in gynecologic procedures [5] and in the setting of obstetric procedures, including Cesarean deliveries [3,4].
In one study using the barbed suture in laparascopic myomectomy
(n=138), the use of barbed suture demonstrated a significant reduction
in mean duration of surgery and length of hospital stay, without
significant differences in peri-operative complications and blood loss
with the use of the barbed suture [1].
In contrast, while other studies found no significant reduction in
total operative time, there was significant decrease in suturing time
and blood loss [6,7].
With respect to those undergoing laparoscopic hysterectomy with and
without robotic-assistance, the use of the barbed suture to close the
vaginal cuff was also associated with a decrease in total operative
time, blood loss, and length of hospital stay without increasing
complications [8,9] and significantly reduced postoperative vaginal bleeding and vaginal cuff dehiscence [10].
In the obstetric world, there has only been an
isolated study regarding the use of the UBS during open surgery. Its use
for dermal closure during Cesarean section was not associated with any
significant differences with respect to incisional cosmesis, dermal
closure time, and wound complications [3].
Our study is novel as it evaluated the use of barbed suture for closure
of the entire Cesarean defect. Overall, there were no differences noted
with respect to overall complications, blood loss, and operative time.
Our results should be interpreted with caution as
there are several limitations including the retrospective design and our
sample size did not provide adequate power to detect a difference in
complication rates. Based on previous work of non-inferiority of 10% of
UBS compared to CBS [3],
our sample size provided 30% power to detect a difference and would
have required 572 patients in each group to provide a power of at least
80%. Regardless, our study demonstrates the technique of using the V-loc
suture in cesarean section is being similar to more conventional suture
types. Lastly, our study only followed outcomes for 6 weeks postpartum;
as a result, long-term outcomes (such as scar formation, strength of
the hysterotomy incision in subsequent pregnancies, and any
unintentional effects on future fertility) with the barbed suture were
not addressed.
A strength of our study is that all the Cesarean
sections were performed or supervised by a single surgeon, minimizing
operator variability and eliminating intervention bias. The difference
in number between the subjects in which the V-loc was used compared to
the number of more CBS used can be explained mostly by surgeon
preference and using a single surgeon’s patient group.
The potential benefits associated with the barbed
suture include a looped or tabulated end, eliminating the need for
knot-tying to secure the suture. Additionally, the suture is created by
cutting barbs into the suture at equal distances, allowing the suture to
self-anchor as it is passes through the tissue. This fixation prevents
the suture from migrating and creates equal tension along the suture
line, creating the effect of a continuous interrupted suture line, but
without requiring multiple knots to be tied to achieve this security.
The barbed suture is also monofilament, which may decrease the incidence
of infection when compared to braided suture.
Conclusion
Our results suggest similar risk profiles using UBS
compared CBS closures and may be considered as an adjunctive suture for
closure of the hysterotomy, fascia and skin during Cesarean section
based on the similar safety and efficacy between the suture types. Our
study adds to the growing body of work on the barbed suture, though
further studies including randomized trials would need to be performed
to better evaluate the efficacy and safety of this method of closure as
well as a cost analysis should also be considered.
Declaration
Ethics approval and consent to participate:
This study was approved by the Wright State University, Miami Valley
Hospital and United States Air Force Institutional Review Boards
Availability of data and material:
The data that support the findings of this study are available from Dr.
Keith Watson but restrictions apply to the availability of these data,
which were used under license for the current study, and so are not
publicly available. Data are however available from the authors upon
reasonable request and with permission of Dr. Keith Watson.
Author’s contributions
Vivina Napier, M.D. - Primary role in study design, data interpretation, and manuscript writing.
Rachel Warwar, M.D. - Data collection and manuscript writing and editing.
Keith Watson, M.D. - Surgeon performing Cesarean sections; provided charts for data collection.
Logan M. Havemann BS – Manuscript writing and editing.
Austin Findley, M.D. – Manuscript writing and editing.
Rose A. Maxwell, PhD – Study planning and statistical analysis.
Steven R. Lindheim, M.D. MMM – Primary role in study planning, data interpretation, and manuscript editing.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment