Juniper Publishers: Huge Brenner’s Tumour of Ovary (6.2kg) in a Postmenopausal Female - a Rare Case Report and Review of Literature
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Rajshree Dayanand Katke*
Transitional cell tumors of the ovary, described for
the first time by Brenner in 1907, are one of the rare neoplasms of all
ovarian tumors and account for nearly 2%. Transitional cell tumors, in
turn, include two distinct clinico-pathological subtypes: Transitional
cell carcinomas (TCCs) and Brenner Tumors [1].
The World Health Organization (WHO) classifies Brenner
tumors into three categories: benign, borderline and malignant.
Borderline Brenner tumors, usually associated with a benign Brenner
tumor, are characterized by papillary structures with a fibro-vascular
core covered by a transitional epithelium. In 30% cases Brenner tumour
is associated with mucinous or serous cystadenoma. We report the case of
a 68-year-old woman with a left ovarian mass, for which the morphology
and histopathological analysis was consistent with the diagnosis of
Brenner tumor associated with mucinous cystadenoma.
Keywords: Transitional cell tumors (TCCs); Brenners tumor; Mucinous cystadenoma; Histopathology; World Health Organization (WHO) Introduction
Brenners tumors are subgroup of transitional cell
tumors. They are generally unilateral, only 5-7 % cases are bilateral.
Sometimes brenners tumor is associated serous or mucinous cystadenomas.
They are usually asymptomatic, may be diagnosed as an incidental
finding. When associated with cystadenomas, they may present as large
ovarian masses which may present mainly with the pressure symptoms over
the genitourinary system leading to urinary complaints and also pressure
over respiratory system leading to respiratory embarrassment [2].
It is generally accepted that Brenner tumors are
derived from the surface epithelium of the ovary or the pelvic
mesothelium through transitional cell metaplasia to form the typical
urothelial-like components. Brenners tumor is a histopathological
diagnosis. Microscopically it is characterised by abundant dense fibrous
stroma with epithelial nests of transitional cells with coffee bean
shaped nuclei resembling those lining the urinary bladder. Surgical
resection of the tumor mass is diagnostic as well as curative for this
tumor.
Case Report
A 67 year old postmenopausal multiparous female
presented to our hospital with complains of pain in abdomen since 1
month and distension of abdomen since 6 months. Patient was a known case
of hypertension and hypothyroidism and was under treatment for the
same. On examination her vitals were stable and no abnormality detected
on general and systemic examination. Per abdominal examination revealed a
mass of around 32 weeks size gravid uterus. It was firm to cystic in
consistency with smooth surface and restricted mobility arising from
pelvis and extending upwards to xiphisternum. On per speculum
examination revealed cervix and vagina healthy.
On per vaginal examination mass of 32 weeks size
felt, origin of which could not be detected. Ultrasonography showed a
complex multicystic mass of 25x11x10 cm arising from left ovary, uterus
and right ovary were normal. Magnetic Resonance Imaging revealed complex
left ovarian neoplasm with enhancing solid and peripherally enhancing
cystic components measuring 25.3cmx16.9cmx10.5 cm with minimal sfree
fluid and no lymphadenopathy.
Tumour markers showed CA 125 level was mildly raised
and was 96.76Iu/ml, CEA and AFP level were within normal limits.
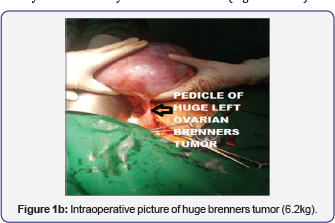
Exploratory laparotomy was done which showed a huge left ovarian cystic
mass of size 25cmx18cmx15 cm, rest of abdominal and pelvic organs were
normal. In situ findings were revealed huge Left ovarian mass of size 32
weeks gravid uterus, huge one soft to firm in consistency with smooth
surface without any surface excreations. Removal of huge left sided
ovarian tumour done after dissection of ureters to avoid damage.to it.
Total abdominal hysterectomy and Right salpingoophorectomy was done. Cut
section showed a cystic mass filled with mucinous material with solid
components. Frozen section suggested a diagnosis of mucinous cystadenoma
with Brenner components.
Microscopic examination revealed a cyst lined by a
single layer of non-ciliated columnar epithelium without stromal
invasion and solid component showed nests of ovoid to polygonal
transitional cells like epithelium and have pale cytoplasm and oval
nuclei. Final Histopathology report confirmed the diagnosis of mucinous
cystadenoma with Brenner component. Post operative period was uneventful
and patient was discharged in Healthy condition. On follow up patient
recovered well and resume the activities.
Discussion
Brenner tumor of ovary is a solid ovarian tumor that
is generally asymptomatic. Although they are predominantly solid on
imaging and pathologic examination, association with serous and mucinous
cystadenomas is up to 30% [3].
It is usually an incidental pathological finding. Among symptomatic
patients, common symptoms include vaginal bleeding, a palpable pelvic
mass, and pelvic pain. Most of the time it is found to be unilateral.
Bilaterality is seen only in 5-7% of the cases. It is generally accepted
that Brenner tumors are derived from the surface epithelium of the
ovary or the pelvic mesothelium through transitional cell metaplasia to
form the typical urothelial-like components [4].
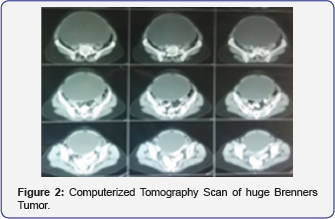
The histological patterns observed in Brenner tumor are typically
benign, with a few reports of borderline or malignant counterparts [4].
It is difficult to diagnose Brenner tumor with imaging studies as the findings are non specific [5].
USG and computed tomography, both the techniques are limited in
specificity because of the tumor’s nonspecific appearance. In imaging
studies benign Brenner tumors are generally similar to those of other
solid ovarian masses such as fibroma, fibrothecoma, and pedunculated
leiomyoma [3].
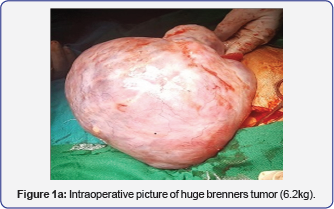
Grossly benign Brenner tumors are well circumscribed,
with a hard or fibromatous, gray, white, or slightly yellow cut
surface. Occasionally the tissue becomes gritty because of calcific
deposit. Borderline Brenner tumors are characteristically cystic and
unilocular or multilocular with cauliflower like papillomatous masses
protruding into one or more of the locules. Malignant Brenner tumor may
be solid or cystic with mural nodules; they usually do not have any
distinctive features (Figure 1a&1b).
Microscopically, they are made of abundant dense
fibrous stroma with epithelial nests of transitional cells resembling
those lining the urinary bladder. The fibrous component is less
prominent in borderline or malignant tumors than in benign lesions.
Complex cystic tumors contain varying amounts of stroma and are more
commonly found with borderline or malignant histologic findings, often
in the form of papillary solid projections within a cystic mass.
Immunohistochemistry and molecular analysis is
helpful in diagnosis and confirmation of Brenner tumour but considering
high cost is not of much clinical value. Borderline Brenner tumors are
negative for p16, Rb and p53, and show weak immunostaining for Cyclin
D1, moderate for Ras and strong for EGFR. They also express p63, as in
benign subtypes but not in malignant ones, and present a diffuse
staining for CK7, CA125, thrombomodulin and EMA, as in all subtypes of
Brenner tumors [1]. Malignant Brenner tumor is also negative for p16, Rb and p53, but strongly positive for EGFR, Cyclin D1 and Ras (Figure 2).
Conclusion
We hereby present a rare case of a huge brenners
tumor of 6.2 kg which presented in a postmenopausal female.
Histopathological examination is most important in diagnosis of Brenner
tumour apart from radiological investigations and immunohistochemistry.
Most Brenner tumors are candidates for surgical resection. Surgical
resection is often diagnostic as well as curative and will reverse
symptoms if they are present.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment