Juniper Publishers: Success of VBAC in a Tertiary Hospital
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Uma Pandey
Abstract
Objectives: To assess success of vaginal birth after caesarean section and maternal-fetal outcome in such cases.
Methods: Prospective Observational
study in a University teaching hospital at Varanasi. The study period
was June 2015-December 2015, a total of 68 patients were included. Those
women who had Caesarean sections in past and were found suitable for
VBAC were included in the study admitted to the labour ward.
Results: 42(61.76%) of women had
VBAC (Vaginal Birth After Caesarean section) and 26 (38.23%) had ERCS
(Emergency Repeat Caesarean Section). Maximum number of women who had
VBAC has LSCS (Lower Segment Caesarean Section) in the past for fetal
distress (73.33%). ERCS (failed VBAC) was done maximally for fetal
distress (53.84%), then for failure to progress (38.46%) and 7.6% for
scar tenderness. Maternal complications were lower in the VBAC group:
fever (9.5%), blood transfusion (7.1%); while ERCS group had wound
infection (30.76%), blood transfusion (34.61%).
Conclusion: The study shows encouraging result for VBAC in a good set up to be followed to reduce Caesarean rate.
Keywords: Vaginal birth after caesarean section; lower segment caesarean section; Uterine rupture; Maternal morbiditiesIntroduction
Planned VBAC is appropriate for and may be offered to
the majority of women with a singleton pregnancy of cephalic
presentation at 37+0weeks or beyond who have had a single previous lower
segment caesarean delivery, with or without a history of previous
vaginal birth [1].
VBAC (Vaginal Birth After Caesarean section) is a
recommended after one Caesarean section, but preferably not after second
Caesarean section as it increases maternal morbidity and mortality.
VBAC conducted in an equipped set up reduces both maternal morbidity and
mortality compared to LSCS (Lower Segment Caesarean Rate). Globally the
rate of Caesarean section is rising and VBAC is a good approach to
reduce the LSCS rate [2,3].
The rates of LSCS are rising all over the world and
also in India. But being a low resource country patients are not able to
afford without stretching their limits. Whilst vaginal delivery has
less chances of infection, no need for General Anaesthesia or Spinal
Anaesthesia, early ambulation and early discharge, better bonding and
breastfeeding [4].
Success of VBAC is 72-75%. Women should be informed
that planned VBAC is associated with an approximately 1 in 200 (0.5%)
risk of uterine rupture. Women should be informed of the two- to
three-fold increased risk of uterine rupture and around 1.5-fold
increased risk of caesarean delivery in induced and/or augmented labour
compared with spontaneous VBAC labour [1,5,6].
UK NHS hospitals have caesarean rate of approximately
25%, while in most American the rate is approximately 50%. This is
usually due to women’ expectations, cultural beliefs, birth plan, fear
for baby with cerebral palsy etc [7].
There is a growing concern over the rising Caesarean
rate across the international borders. Increased caesarean leads to
gynaecological as well as obstetrical problems. Gynaecolgical:
infertility, recurrent abortions, difficult hysterectomy due to bladder
adhesions; Obstetrical:placenta percreta, placenta praevia, peripartum
hysterectomy, peripartum cystectomy and maternal death due to torrential
blood loss [8].
Caesarean section leads to more maternal morbidity
and mortality than normal delivery, although caesarean section may be
safer than normal vaginal delivery for the baby. Sometimes the families
are poor and can’t afford caesarean. In primary health centers there may
not be facilities available for fetal monitoring or anesthesia and
there is lack of trained personnel.
We wanted to study maternal and fetal outcome in
cases of vaginal birth after caesarean section in a tertiary health
center of north India.
Methods
This prospective observational study was done at Sir
Sunder Lal Hospital, Banaras Hindu University, Varanasi, India. This
University teaching hospital is a tertiary referral centre for most of
the Eastern Uttar Pradesh, Bihar, Jharkhand, parts of Odisha and MP
states of India. The hospital is a referral center for high-risk
pregnancy and critically ill obstetric cases. The per annum delivery
rate is approximately 1,500 with a high caesarean rate of 52%.
The study period was June 2015-December 2015, a total
of 68 patients were included. Those women who had Caesarean sections in
past and were found suitable for VBAC were included in the study
admitted to the labour ward.
Inclusion criteria
- Non-recurrent indication for previous LSCS
- Lower Segment Caesarean Section
- Adequate pelvis
- Cephalic presentation
- No Medical complications
- No Obstetrical complications
Exclusion criteria
- H/O Classical Caesarean
- H/O inverted T uterine incision
- H/O uterine rupture
- Contracted pelvis
- Twin gestation
- Macrosomia
- Shortened inter-delivery interval
- Medical complications
- Obstetrical complications
All participants were counseled adequately regarding
the success, maternal and neonatal complication rate. RCOG guideline was
followed “Women considering their options for birth after a single
previous caesarean should be informed that, overall, the chances of
successful planned VBAC are 72–76%. All women who have experienced a
prior caesarean birth should be counseled about the maternal and
perinatal risks and benefits of planned VBAC and ERCS when deciding the
mode of birth”.
Participants’ consent was obtained. Data collection
was done on a proforma. Data obtained included age, parity, history of
previous normal delivery or caesarean section (indication, was it
classical, infection after caesarean). Mode of delivery in current
pregnancy, was the labour spontaneous, induced or augmented, episiotomy
infection, Indication of Lower Segment Caesarean Section (LSCS), wound
infection. Peroperative or preoperative diagnosis of uterine dehiscence
or uterine rupture? Baby details eg weight and apgar score at birth was a
also noted. Maternal satisfaction score, quality of life score and cost
score was also noted.
Labour was monitored as per protocol. All
participants were followed through delivery and for the postpartum
period. Main outcome measure was outcome in the index pregnancy while
secondary outcome measures were maternal and neonatal outcome.
Results
Total 68 patients were recruited and thoroughly
counseled. They were included if they satisfied the inclusion criteria
for VBAC trial. All patients had spontaneous onset of labour. The age
range of the parturient was 19-27 years.
History of SVD (Spontaneous Vaginal Delivery) was
present in only 12 pregnant mother, they had a normal delivery before
LSCS (Lower Segment Caesarean Section). These women had successful VBAC
in our study.
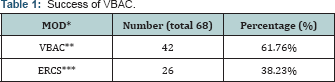
*Mode of delivery
**Vaginal Birth after Caesarean section
***Emergency Repeat Caesarean Section
42 (61.76%) of women had VBAC (Vaginal Birth after
Caesarean section) and 26 (38.23%) had ERCS (Emergency Repeat Caesarean
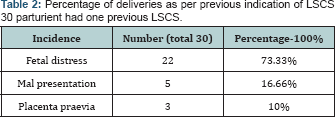
Section) (Table 1). Maximum number of women who had VBAC has LSCS (Lower Segment Caesarean Section) in the past for fetal distress (73.33%) (Table 2).
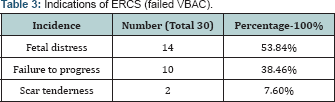
ERCS (failed VBAC) was done maximally for fetal distress (53.84%), then
for failure to progress (38.46%) and 7.6% for scar tenderness, (Table 3).
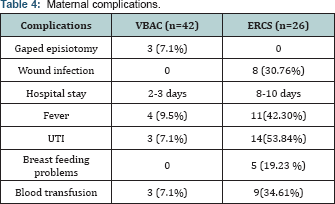
Maternal complications were lower in the VBAC group:
fever (9.5%), blood transfusion (7.1%); while ERCS group had wound
infection (30.76%) and blood transfusion (34.61%), (Table 4).
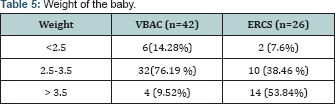
There were 76.19% of babies in VBAC group who weighed 2.5-3.5 kg, while > 3.5 kg babies were 53.84% in the ERCS group, (Table 5).
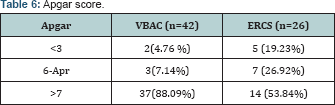
Babies born by ERCS who had Apgar <3 were 5/26 (19.23%) suggest that
LSCS in certain cases of failure to progress may not give maternal or
fetal outcome like Elective Caesarean section.
There was no case of classical caesarean section in
the past or history of sepsis in the previous pregnancy. Induction or
augmentation of labour was not done in any case. There was no incidence
of scar dehiscence or uterine rupture in our study.
The maternal satisfaction score was 6-8/10; quality
of life score was 5-7/10. But, the cost score was 3-5/10 in our study.
This suggests that most pregnant women are satisfied with our services
but the cost of the treatment is a bit too much for them to bear (Table 6).
Discussion and Conclusion
The success of VBAC is 61.76%, which is similar to other studies [9,10].
Maximum number of women who had VBAC has LSCS (Lower Segment Caesarean
Section) in the past for fetal distress (73.33%), shows that VBAC is
more successful in this kind of non-recurrent indication. Maternal
complications were lower in the VBAC group, which also favors the notion
of promoting VBAC in the antenatal plan if deemed suitable.
The above study shows that VBAC is lesser maternal
morbidity than ERCS and hospital stay is also less. So, if VBAC is done a
center which is well equipped with fetal monitoring, maternal
monitoring and has the facility for emergency operation then it should
be mode of delivery of choice.
ith increasing Caesarean rate maternal long-term
complications also increase. Therefore we should endeavor towards
encouraging women to have VBAC while ensuring fetal and maternal safety.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on:https://juniperpublishers.com/jgwh/




Comments
Post a Comment