Juniper Publishers: Venous Thrombo prophylaxis in Pregnancy and Puerperium: the Saudi Algorithm
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Hisham Arab*
Adequate use of venous thromboembolism (VTE)
prophylaxis is considered an indicator of quality of care in any medical
institution. However, like in many other countries, we found out that
in Saudi Arabia around 50% of Obstetric patients failed to get
thromboprophylaxis when it was indicated, and the main reason was
physicians overlooked performing the thromboembolism risk assessment.
Accordingly, many measures took place in our health system over the past
few years, including increasing doctors and patients' awareness,
improving admission protocols, and simplifying the risk assessment
procedure for a busy practitioner. 9 experts from around the country
reviewed all published international guidelines on this subject, and
came up with an algorithmic approach with the recommended prophylactic
measure for any patient at a glance. By excluding the past history of
thromboembolism and/or Thrombophilia which is very rare among our
pregnant patients at booking (<1%), attention will be directed to one
page algorithm that covers all other possibilities whether antenatal or
postnatal, with the recommended measure of thromboprophylaxis. A word
of caution, complicated cases or conditions that require the use of
anticoagulant other than low molecular weight heparin (LMWH) should
consult a thrombosis specialist or refer to major guidelines.
Abbreviations: VTE: Venous Thromboembolism; LMWH: Low Molecular Weight Heparin; CASP: Critical Appraisal Skills Programme; PGM: Prothrombin Gene Mutation; UH: Unfactionated Heparin; ACOG: The American Congress of Obstetricians and Gynecologists; SOGC: The Society of Obstetrician and Gynecologist of Canada; RCOG: The Royal College of Obstetricians and Gynecologists; ACCP: American College of Chest Physician
Introduction
Venous thromboembolism (VTE) considered one of the
leading causes of maternal morbidity and mortality all over the world.
The reported incidence of VTE from most developed countries ranging
between 1-2 cases per 1000 pregnancies [1]. The risk of deep venous thrombosis is five times higher comparing to non pregnant women [2].
The risk of VTE is greater in postpartum than during the antenatal
period. Deepvein thrombosisin pregnant women occurs more frequently in
the left leg (85%, vs. 55%) among nonpregnant [3].
Searching in the literature, there is very limited data about the
incidence ofVTE in pregnancy and puerperium in Saudi Arabia. The
reported study from Saudi Arabia showed that the incidence of VTE is
1.25 cases per 1,000 deliveries (95% CI 0.89-1.16) [4].
The Maternal mortality rate was 0.02 5 case per 1,000 deliveries.
Exploring the risk factors to develop VET that was described in
different guidelines showed that the majority of obstetrical population
in our society is considered as high risk. These risk factors included
but not limited to, multiparity, obesity, advanced maternal age repeated
cesarean section and consanguinity marriages which may increase the
risk of inherited thrombophilia thereby increasing risks of VTE. The
above mentioned fact made it essential to develop tailored guidance to
our high risk obstetrical population compared to the developed
countries.
Admitting that the incidence and the mortality rate
are under estimated in the face of lacking postmortem autopsy to confirm
the diagnosis of suspected death related to VTE and that we need more
work to determine our own incidence and risk factors. This algorithm was
developed based on the best available data and international guidelines
to date. The aim of this algorithm is to help the health care providers
across the Kingdom of Saudi Arabia in implementing systematic and
simplified approach towards the prevention and management of VTE during
pregnancy, labor and puerperium.
Methodology
The development group for these guidelines consists
of a panel of Maternal-Fetal Medicine experts in different sectors in
the medical care system in the kingdom of Saudi Arabia including
National Guard, military, universities, ministry of health and private
sector.
Literature search was carried out at the following
electronic databases: The Cochrane Library (including the Cochrane
Database of Systematic Reviews, the Cochrane Central Register of
Controlled Trials and the Database of Abstracts of Reviews of Effects
[DARE]), EMBASE, the ACP Journal Club, PUBMED,
Medline, (CDSR), Journal full text via OVID search engine and Science
Direct.
The databases were searched using the relevant
Medical Subject Headings (Mesh) terms, including all subheadings. The
principal search terms used were: 'venous thromboembolism',
'thrombosis', 'pregnancy', 'postpartum', 'puerperium', 'antenatal',
'prenatal'. The search was limited to humans and the English language.
In addition, the reference lists of studies selected
for inclusion were scanned for relevant studies. Guidelines on venous
thromboprophylaxis in pregnancy and puerperium from different well
recognized health care institutions and organization including: The
American College of Obstetricians and Gynecologists (ACOG) [5,6], The Society of Obstetrician and Gynecologist of Canada (SOGC) [7], The Royal College of Obstetricians and Gynecologists (RCOG) [8,9], American College of Chest Physician (ACCP) [10], The Australian [11] and The Irish [12] were reviewed.
Due to the lack of evidence in thromboembolic events
among pregnant women in Saudi Arabia a pilot data collection study
performed in the city of Medina to compare the prevalence and the risk
factors of VTE among pregnant Saudi women with data reported in the
literature.
The targeted clinical questions were divided into
tasks, which were distributed among the committee members; each member
was assigned individual topics. On completing the task the assigned
member was asked to present the results of his work to the group to be
appraised by workgroup members using Critical Appraisal Skills
Programmed (CASP) checklist [13].
This working group has concluded that they are in
agreement with the classification of evidence level and the grade of
recommendation presented in the Green-top Guideline No. 37a April 2015
of the RCOG. Hence, for this purpose readers are referred to this
guideline.
A comprehensive summary of this group's
recommendations for VTE thromboprophylaxis in pregnancy and puerperium
is the mainstay of this document followed by an appendix of quick
reference algorithm to simplify this task for the busy clinician.
Risk Assessment and Thromboprophylaxis Recommendations
There are certain factors that determine the
magnitude for the risk of VTE in association with the pregnancy or the
puerperium. These are called risk factors that have been identified
after an extensive literature search and presented recently in 2 major
guidelines published from Canada (2014) and United Kingdom (2015).
After establishing the characteristics of the Saudi
reproductive performance and their VTE risk factors, the reviewers
critically analyzed those international guidelines, and developed their
expert opinion of the best applicable thromboprophylactic
recommendations for this population as outlined in this review.
Risk Assessment is a dynamic process that should be
carried out on the first pregnancy visit and repeated whenever there was
any development or admission during the course of pregnancy, during
labor, and immediately after delivery.
The Algorithm
We have identified 2 major personal risk factors and they
are:
- Personal history of previous VTE
- Personal history thrombophilia
The incidence of these 2 personal risk factors is
<1%. Hence, it would be much easier during risk assessment process to
exclude these 2 conditions from the beginning by using Algorithm 1
first (Figure 1).
On this algorithm, the health care provider will find the recommended
Thromboprophylaxis measure according to the patient situation.
Regardless of any risk factor, the personal history
of previous VTE or thrombophilia is an independent factor that dictates
its prophylactic measures in a pre-conceptional counseling assessment or
anytime the patient found to be pregnant.
Situation 1
Previous history of VTE due to thrombophilia:
Whether it was a heritable (antithrombin deficiency) or an acquired
(antiphospholipid syndrome) thrombophilia, these patients are often on
long term oral anticoagulants and a hematologist should be involved in
their thromboprophylaxis management. High dose of LMWH (50-75% of the
therapeutic dose) should be recommended throughout the antenatal period
and for 6 weeks postpartum. Then, they should go back to their
pre-pregnancy treatment modality.
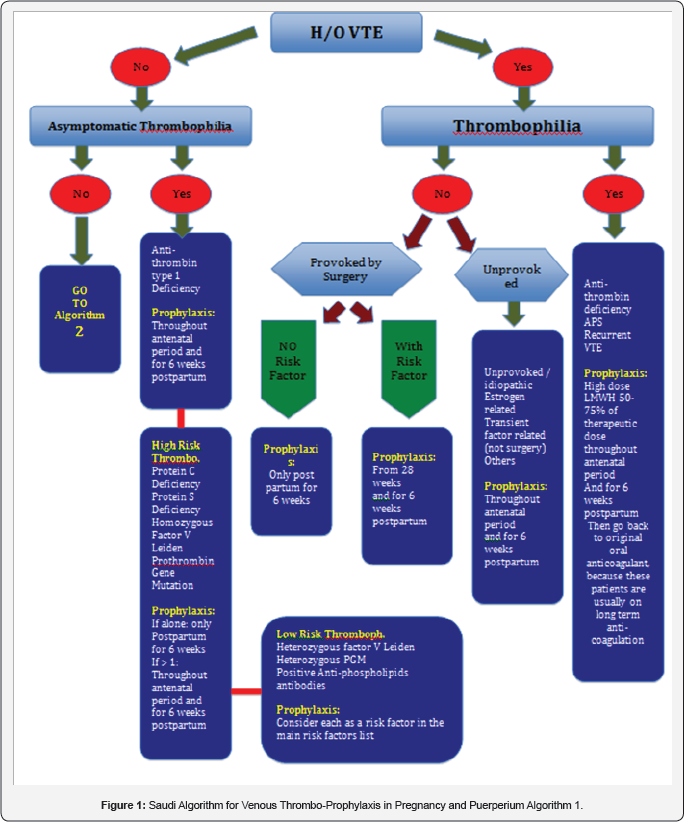
Situation 2
Previous history of VTE without thrombophiliaIf the
VTE was unprovoked, i.e. idiopathic, estrogen related, or due to
transient factor not related to surgery, patient should have
thromboprophylaxis throughout the antenatal period and for 6 weeks
postpartum. If the VTE was provoked by surgery, then Risk Factors from (Table 1 & 2)
should be explored: in the absence of risk factors then prophylaxis is
limited to the 6 weeks postpartum period. However, the presence of any
risk factorin this situation would require thromboprophylaxis commenced
at 28 weeks gestation and continued for 6 weeks postpartum.
Situation 3
Asymptomatic thrombophilia is present but no previous history of VTE:
Thromboprophylaxis depends on the type of the thrombophilia
Thromboprophylaxis is recommended throughout the antenatal period and
for 6 weeks postpartum.
Anti-thrombin type I deficiency: Thromboprophylaxis is recommended throughout the antenatal period and for 6 weeks postpartum.
High risk thrombophilia: such as protein C deficiency, protein S deficiency, Homozygous Factor V Leiden and Prothrombin Gene Mutation (PGM):
- If more than one are co-existing, the prophylaxis will be similar to antithrombin deficiency
- However, if only one exists, the recommended prophylaxis will be limited to the 6 weeks postpartum period.
Low risk thrombophilia: such as heterozygous
factor V Leiden, Heterozygous PGM, or positive anti-phospholipids
antibodies: Thromboprophylactic recommendation is to consider each one
of the above as a risk factor added to Table 1 & 2 and act according to recommended management of using such tables.
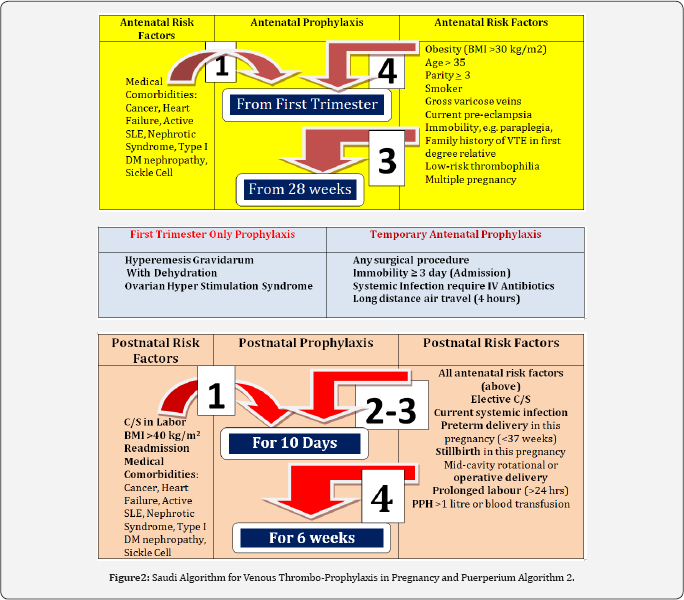
Situation 4
thrombophilia: This constitutes the vast majority of
our patients and their thromboprophylactic management depends on risk
factors that are grouped in ( Tables 3),
namely: Antenatal, postnatal and transient. According to the number of
risk factors present from any of the tables the recommended
thromboprophylactic measure is stated at the end of the arrow. This
Tables 3 are grouped in one page and collectively called Algorithm 2 ( Figure 2).
Antenatal thromboprophylaxis ((Table 1)
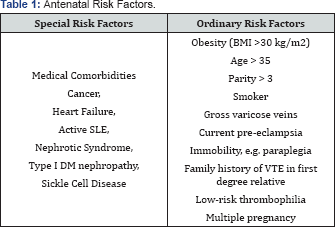
- In the presence of any Special antenatal risk factor, prophylaxis should be started from the first trimester.
- In the presence of four (4) Ordinary risk factors, prophylaxis should also be started from the first trimester.
- In the presence of three (3) Ordinary factors, prophylaxis should be started from 28 weeks.
- In the presence of one or two (1 or 2) Ordinary risk factors, no antenatal thromboprophylaxis is needed.
Postnatal thromboprophylaxis: (Table 2)
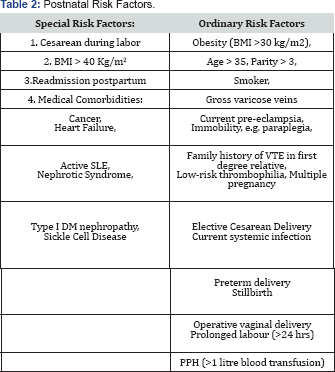
- In the presence of any Special antenatal risk factor, prophylaxis should be started from the first trimester.
- In the presence of four (4) Ordinary risk factors, prophylaxis should also be started from the first trimester.
- In the presence of three (3) Ordinary factors, prophylaxis should be started from 28 weeks.
- In the presence of one or two (1 or 2) Ordinary risk factors, no antenatal
Transient (Temporary) thromboprophylaxis: (Table 3)
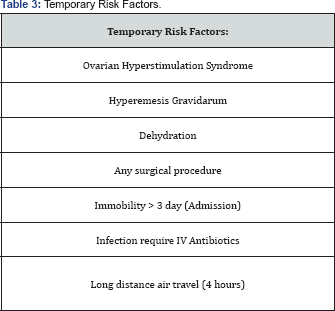
- Any case of ovarian hyperstimulation syndrome that got pregnant should be receiving antenatal prophylaxis throughout the first trimester only
- Temporary thromboprophylaxis is recommended in pregnancy when it is complicated by any of the following: Hyperemesis Gravidarum with dehydration, admission for a surgical procedure, immobility for more than 3 days, systemic infection requiring IV antibiotics, and long distance air travel (> 4 hours).
Thromboprophylaxis during labor and delivery
Women receiving thromboprophylaxis during the antenatal period should:
- Stop further doses if developed vaginal bleeding or labor started.
- Omit morning dose if going for Cesarean section.
- Not have regional analgesia till 12 hours after the last prophylactic dose.
Women who just delivered should receive a VTE prophylaxis:
- Immediately after a normal delivery
- 4 hours after removal of the epidural catheter
- 6 hours after a Cesarean delivery
Choice of Anticoagulant and Dosing
Unfractionated Heparin (UH) and LMWH do not cross the
placenta and do not cause teratogenicity or fetal bleeding. Due to its
lower side-effects profile and ease of dosing and administration LMWH is
recommended over UH for use in pregnancy. The purpose of this
algorithmic guidance is to be simple and direct and hence LMWH is the
only anticoagulant agent referred to for thromboprophylaxis
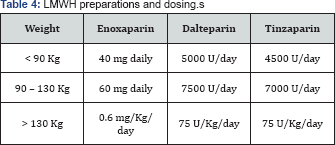
recommendations in this document. Table 4 is showing different dosing schemes based on the patient's pre-pregnancy weight.
Readers are referred to other guidelines for usage of
other anticoagulants. Aspirin should not be used as a VTE
thromboprophylactic agent. Anti-embolism stockings can only be used in
conjunction with anticoagulant prophylaxis.
Conclusion
In order to ensure that all women at risk of VTE are
identified and received the appropriate thromboprophylaxis this quick
and easily glanced algorithm was developed to be utilized by Saudi
health care providers in hospitals and clinics as well as rural areas.
By excluding the past history of thromboembolism and/or Thrombophilia
which is very rare among our pregnant patients at booking (<1%),
attention will be directed to one page algorithm that covers all other
possibilities whether antenatal or postnatal, with the recommended
measure of thromboprophylaxis. A word of caution, complicated cases or
conditions that require the use of anticoagulant other than LMWH should
consult a thrombosis specialist or refer to major guidelines.
Authors’ contributions
The authors had 4 meetings over a one year period to
write the above statements based on published data and to bring their
expertise in the thromboprophylactic management in pregnancy and
puerperium. All authors contributed to the writing and integration of
the different segments of the manuscript. All authors read and approved
the final manuscript.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment