Juniper Publishers: The Diagnosis Challenge of a Case of Spontaneous Heterotopic Pregnancy
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal
of Gynecology and Women’s Health-Juniper Publishers
Authored by Xiping Luo*
Abstract
Heterotopic pregnancy was rare after natural
conception, and easy to be missed or misdiagnosed. We present a case of
spontaneous heterotopic pregnancy, which was diagnosed correctly with
discretion and successfully treated by laparoscopic salpingectomy.
Keywords: Heterotopic pregnancy; Interstitial pregnancy; Spontaneous; Gestational trophoblastic neoplasiaAbbreviations: ART: Assisted Reproductive Technology; GTN: Gestational Trophoblastic Neoplasia
Introduction
Heterotopic pregnancy refers to the simultaneous
occurrence of two or more implantation sites, most of which are
intrauterine pregnancy combined with ectopic pregnancy. Although the
widely spread use of assisted reproductive technology (ART) increased
the incidence of heterotopic pregnancy, it was rare after spontaneous
pregnancy, with an estimated incidence of around 1:30,000 [1].
Few specific symptom or sign exists in early stage of heterotopic
pregnancy, which caused misdiagnosis. Correct diagnose rely mostly on
history, ultrasonography and HCG. Treatment of spontaneous heterotopic
pregnancy includes medical treatment and surgery, while early diagnosis
might avoid serious complications.
Case Reports
A 28-year-old patient presented to the gynecology
department with a history of increasing HCG level at 24 days after
suction of missed abortion. She was diagnosed as missed abortion at 47
days of natural pregnancy with HCG of 6219 IU/L. D & C 2 days later
found obvious villi which was confirmed by histology. The HCG level
decreased to 3888 IU/L at 3 days after D&C, but increased to 8325
IU/L 7 days later. Both transvaginal ultrasound and hysteroscopic
examination found no abnormal sign. On further monitor, the HCG level
kept on increasing. A pelvic MRI examination found no mass in the uterus
or in the abdomen. The patient had no vaginal bleeding or abdominal
pain, and denied sexual life after D&C.
The patient did laparoscopic salpingoplasty before
because of primary infertility, and got pregnancy by IVF-ET, then
delivered a baby by cesarean section 1 year ago because of macrosomia.
But the pregnancy of missed abortion was conceived spontaneously.
Doctors from an oncology center diagnosed as gestational trophoblastic
tumor and suggested chemotherapy. She was reluctant to receive
chemotherapy and referred to our hospital.
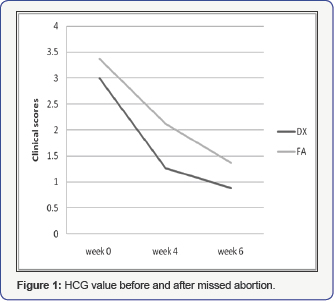
On gynecologic examination, the uterus was in normal
size without any mass in bilateral adnexal area. Transvaginal
ultrasonography was repeated without any positive findings. Both chest
ray and brain CT results were normal. HCG level decreased slowly in the
following days (Figure 1).
Although the abnormal high HCG level after missed abortion supported
the diagnosis of gestational trophoblastic neoplasia (GTN), we supposed
the HCG level should increase more rapidly if it was really a GTN. So we
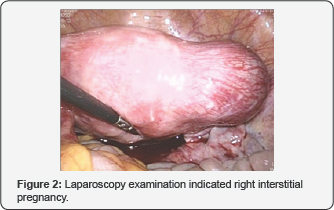
repeated transvaginal ultrasound examination again on 30 days after
D&C, which finally found a 3cm×4cm mass in the right cornua.
Laparoscopy examination confirmed right interstitial pregnancy (Figure 2).
A right-sided salpingectomy was performed. Histology confirmed an
ectopic pregnancy. The patient recovered uneventfully after the
operation.
Discussion
Heterotopic pregnancy was rare. Risk factors of
heterotopic pregnancy include ART, pelvic inflammatory disease, prior
tubal surgery including salpingectomy and reconstructive tubal surgery [2].
Heterotopic pregnancy can have various presentations. It should be considered more likely
- After assisted reproduction techniques.
- With persistent or rising chorionic gonadotropin levels after dilatation and curettage for an induced or spontaneous abortion.
- When the uterine fundus is larger than for menstrual dates.
- With more than one corpus luteum.
- With absence of vaginal bleeding in the presence of signs and symptoms of ectopic gestation and
- When there is ultrasound evidence of uterine and extrauterine pregnancy [3].
Heterotopic pregnancy was easy to be missed or
misdiagnosed. Except the reason of patients who did not visit doctors in
early pregnancy, the main cause might be that gynecologists rely too
much on ultrasound conclusion, while radiologists omit to scan the
pelvic area carefully in the sign of intrauterine pregnancy. In a review
of 82 cases of heterotopic pregnancy, 33% of cases only simply reported
a normal single or multiple intrauterine in a previous ultrasound scan.
However, there was also the possibility that ectopic pregnancy did not
grow as fast as intrauterine pregnancy which made it difficult to
diagnose at early time. In unruptured and ruptured heterotopic pregnancy
after ART, 66.7% and 85.7% cases were diagnosed by ultrasonography
before 7 weeks of pregnancy respectively [4]. To date, there was no similar data concerning natural heterotopic pregnancy.
In our case, ultrasonography and pelvic MRI did not
find the existence of ectopic pregnancy until 79 days of pregnancy. It
might be easy to make a diagnosis of GTN and start chemotherapy in this
case, as high HCG level persisted after missed abortion. Although no HCG
monitoring guideline was recommended in GTN after non-molar pregnancy [5],
from our experience we speculated that HCG should keep on increasing
rapidly instead of slightly decreasing in the last week of surveillance.
Thus, considering the prior tubal surgery history and the trend of HCG
level, we preferred to monitor carefully instead of urgent chemotherapy.
Finally, ectopic pregnancy mass was found. The successful diagnosis
avoided chemotherapy and rupture of ectopic pregnancy at the same time.
Conclusion
Heterotopic pregnancy in natural conception was rare
and had varied presentations. Correct diagnosis demands experienced and
responsible doctors to make. Heterotopic pregnancy must be considered
when HCG level did not decrease as expectantly after D&C for an
abortion. It is possible to monitor the HCG level cautiously instead of
diagnosing GTN and starting chemotherapy in a short time.
Conflict of Interest
The authors report no declarations of interest.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment