Juniper Publishers: Huge Ovarian Mass with Pregnancy: a Case Report from Rural India
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Ekta Singh*
Introduction
The incidence of ovarian tumors in pregnancy is
approximately 1 in 1000, of which 2-5% tumors are malignant (1 in
12,500-25,000 pregnancies) [1].
Among all the tumours diagnosed during pregnancy, the germ cell tumours
reportedly the most prevalent, and epithelial ovarian tumour accounts
for 20% of all ovarian malignancy epithelial ovarian cancers affects
predominantly perimenopausal and post menopausal women [2].
Ovarian mucinous cystadenocarcinoma, a subtype of epithelial ovarian
cancer, is rarely diagnosed during pregnancy in young women. Ultrasound
scanning in pregnancy has lately become a routine. It has led to more
frequent findings of the relatively asymptomatic adnexal masses [3].
In the absence of large prospective randomized trials and cohort
studies, it is difficult to know how best to manage these patients. In
dealing with a pregnant woman with ovarian cancer, one must consider the
effects of the malignancy on the woman and the fetus and how the
pregnancy itself can change the diagnostic procedures and therapy [4].
In spite of all the facility, large ovarian masses
can be detected accidently in rural background as in this case, because
of lack of awareness of routine antenatal checkups in pregnancy. Here we
discuss a rare case of large mucinous cystadenocarcinoma with
undiagnosed live pregnancy of 16 weeks in a 26 years old multi gravida.
Case Report
An unbooked rural woman G4P2L2A1 aged 26yrs presented
herself in our outpatient department with chief complaints of 4 months
amenorrhea along with progressively enlarging large abdominal lump for
last five months and pain in abdomen for 2 days.
On examination her built was average, general
condition was fair with normal vitals. Abdomen was distended with normal
overlying skin. On palpation a non tender firm to hard consistency lump
of about 32 weeks size of gravid uterus with restricted mobility was
found. Lump was non ballot able with reachable Lower pole. A separate 16
wks size mass having firm consistency felt in left iliac fossa Figure1). Per speculum examination did not revealed any cervical or vaginal abnormality.

On sonography 16 weeks intrauterine live pregnancy
with large 18x20cm size solid cystic adnexal mass was diagnosed. There
was no associated ascitis or other pathology detected.
Haematological investigations were found to be within
normal limits. Her CA-125 was 90 m IU which was minimally raised. As
she was already 16 wks pregnant decision for exploratory laparotomy with
conservative surgery was taken. Abdomen was opened by midline
infraumblical incision, no free fluid was found in
peritoneal cavity, left sided twisted ovarian tumour of about 20x16 cm,
along with gravid uterus of 16 wks, was found. Surface was smooth; there
were no adhesions (Figure 2).
Peritoneal washings and omental biopsy were taken. Left sided
cystectomy with salpingo oophrectomy was done. Right sided tube and
ovary seems to be normal. On palpation there was no other pathology
detected. Tissue sent for histopathological examination. Tocolytics were
given to prevent uterine contractions and miscarriage.

Histology reports turned out to be malignant mutinous
cyst adeno carcinoma which was confirmed by IHC (immuno histo
chemistry) test also. According to FIGO staging she belongs to stage-1a
of ovarian carcinoma with pregnancy (Figure 3).
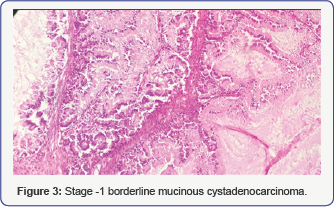
Post operative period was uneventful. As she was
diagnosed as stage-1 borderline mucinous cystadenocarcinoma, decision to
continue the pregnancy and follow up of patient was taken. She is now
36 wks pregnant without any maternal or fetal complications.
There is limited experience of chemotherapy during
pregnancy so we decided to go for chemotherapy if required after
delivery of baby.
Discussion
Fewer than 20% of epithelial ovarian cancers occur in
premenopausal women. However, now ultrasound monitoring is routinely
used during pregnancy, adnexal mass findings in pregnant women are
relatively common [4].
The majority of ovarian cancers associated with pregnancy are diagnosed
at an early stage, when disease is still confined to the ovary [5].
As the incidence of invasive cancers and borderline
ovarian tumours diagnosed during pregnancy is low, treatment strategies
should ideally be discussed and structured during a “multidisciplinary
meeting” involving specialists [6]. Pregnant women with ovarian malignancy should be treated in the same way as nonpregnant women [7].
The second trimester is generally considered as the best time for
surgical intervention because the risk of miscarriage is lower.
Chemotherapy is contraindicated during the first trimester of pregnancy
because of the high rate of abortion and abnormal fetal development [8]. It is not the case during the second or third trimester, but the choice of couple must be considered [4]. Pregnant women in advanced stage of ovarian cancer seems to have poor prognosis.
The optimal surgery for staging ovarian cancer
includes a bilateral salpingo-oophorectomy, total hysterectomy, pelvic
and para-aortic lymphadenectomy, and omentectomy. An analysis of studies
of the medical and surgical management of ovarian carcinoma during
pregnancy showed that the primary surgery at diagnosis consisted of an
ovarian cystectomy, unilateral salpingo-oophorectomy (USO) only, USO
plus multiple biopsies or USO plus more radical surgery as infracolic
omentectomy, appendectomy, peritoneal biopsies, and even pelvic and
para-aortic lymphadenectomy [9].
In case of suspected low malignant potential ovarian
mass on laparotomy, if facility of frozen section is not available as in
our case, treatment can be conservative by adenexectomy and peritoneal
cytology and exploration with biopsies. The treatment should be
performed without rupture by a surgeon/anaesthetist team trained to such
oncologic surgical procedure in pregnant patients. A super conservative
treatment (cystectomy alone) should only be indicated in a patient with
one ovary or with a bilateral borderline tumour. If this borderline
tumour is revealed by the histology of a surgical specimen as in our
case, it seems reasonable, considering the good prognosis of these
tumours to defer surgical treatment until after delivery. Surgical
staging should be completed 3 to 6 weeks after delivery along with or
without chemotherapy [6].
Conclusion
In spite of a lot of advancement in medical sciences few rural areas are even today suffering from lack of basic health facilities need consideration.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Nice share! Thanks a lot for such a lovely blog posting this time around as well.Best Fertility Centre
ReplyDelete