Juniper Publishers: Lipshütz Ulcer: An Undiagnosed Entity
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by A Kovaleva*
Abstract
Lipschütz ulcer is a rare cause of vulvar ulcerous
diseases and it is often underdiagnosed, probably because of the lack of
knowledge about this diagnosis. The aim of this article is to review
the pathogenesis, clinical presentation, differential diagnosis and
management of this entity.
Keywords: Lipschütz ulcer; Epstein-Barr virus; PainIntroduction
Lipschütz ulcer is an entity that occurs in sexually
inactive young women. The typical presentation in the emergency
department is a healthy teenage girl with a first episode of painful
vulvar lesion preceded, generally, by a flu-like syndrome a few days
before.
Discussion
Lipschütz ulcer was firstly described in 1912 by
Benjamin Lipschütz, and it is also known by “ulcers vulvae acutum”. It
mainly affects non-sexually active adolescents and young adults, but
there are even reported cases in children under two [1].
The precise incidence is unknown, and it seems to be a
rare condition, probably because it is greatly under-reported and many
cases are misdiagnosed with other vulvar ulcerous diseases.
The exact pathogenesis is still unclear. One
hypothesis suggests that the ulcer is a clinical manifestation of a
hypersensitivity reaction to a distant viral or bacterial infection,
such as the Epstein-Barr virus infection [2].
The causative agent might reach the vaginal mucosa and disturb the
microbiota, turning the Döderlein lactobacilli into pathogenic species [3].
Although the ulcers are not infectious or sexually
transmitted, a case of Lipschütz ulcer in twin sisters with a probable
airborne infectious transmission has been reported [4].
The diagnosis is usually made by exclusion of other
common causes of genital ulcerations. The first step is to be aware of
the existence of this entity. The physical examination shows a single or
multiple ulcers, with an overlying yellowish-grey exudate and raised
borders on labia minor or major, very painful to the touch. Bilateral
‘Kissing lesions’ are characteristic [5].
A very detailed anamnesis must be carried out to find out a possible
recent history of upper respiratory tract infections, among other
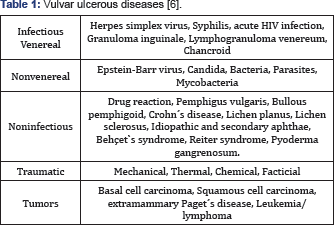
important aspects. The differential diagnosis to consider includes
sexually and non sexually transmitted infections, autoimmune conditions,
drug reactions and local manifestations of systemic illness [6]. It can also be confused with sexual abuse, leading to unnecessary investigations and anxiety to the family [7].
- First episode of acute genital ulceration.
- Being younger than 20 years.
- Presence of one or multiple deep, well delimited, painful ulcers with a necrotic base on the labia minor or major.
- Bilateral “kissing” pattern.
- Absence of sexual contact during the past 3 months.
- Absence of immunodeficiency.
- Acute course of the genital ulcer (abrupt beginning and healing without scarring within 4 to 6 weeks).
The complementary tests should include a viral
culture or PCR for HSV and a serological test for EBV. Other tests will
be performed upon clinical suspicion. The biopsy is not necessary, but
if the ulcer is persistent, it may be helpful (Table 1).
In most cases, the ulcer heals
spontaneously within four to six weeks. The treatment is mainly
supportive and should include pain relief and topical treatment of the
lesion. Empiric treatment will include analgesics and topical
anaesthetics, as well as sitz baths. In case of severe pain,
hospitalization is indicated. If urination is very painful permanent
catheterization should be considered [8]. Use of systemic corticoids and broad-spectrum antibiotics can be indicated in severe cases.
Conclusion
Lipschütz ulcer is often under diagnosed and mistaken
with other vulvar ulcerous diseases. It must be considered in young
virgin patients with painful necrotic ulcers and a history of a recent
viral or bacterial infection. Keeping in mind this diagnosis should
avoid unnecessary treatments to the patients, since it is a
self-limiting disease.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment