Juniper Publishers: Sperm Agglutination, Sperm Shaky Head Movement and Sperm-Cervical Interaction Tests could be enough for Diagnosis of Immunological Infertility?
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Ahmed K Allow*
Abstract
Objectives of this work were: 1) to investigate the
infertile patients with immunological infertility through the assessment
of their results of semen analysis, sperm agglutination (SA) and sperm
shaky head movement (SSM). 2) Study the recovery of sperm-cervical mucus
interaction in infertile couples was studied. Patients and Methods: two
hundred and eight infertile couples were investigated. Female factor of
infertility was normal. According to the percentage of SA patients were
divided into 2 groups. Patients also were studied according their age
factor to three age groups. The sperm-cervical mucus interaction was
studied. Results: The seminal fluid infection was recorded as the higher
percentage of causes of infertility in patients group-I in compared to
patients in group-II. SA was noted significantly (P=0.002) higher in age
group 2 (30-40 years) compared to age group 1 and 3. Percentage of SSM
was significantly, P=0.03, in the age group 3 compared to age group 2.
The percentage of motility of sperm recovery was significantly better in
age G2 compared to age G1 and 3. At the same time the heist sperm
concentration recovery as well as sperm agglutination were significantly
(p=0.02) higher in age group 2. Conclusion: 60% of causes of
immunological infertility mainly associated with sterile seminal fluid
infection. The SA and SSM should be involved as routine tests to
diagnose of immunological infertility. Percentage of SSM was increased
by an increment in the age of patients.
Keywords: Sperm agglutination; Immunological infertility; Yemeni infertile couplesIntroduction
Conception is normally achieved within twelve months
in 80-85% of couples who use no contraceptive measures and persons
presenting after this time should therefore be regarded as possibly
infertile and should be evaluated. Immunologic factors are considered as
important causes of infertility [1].
One of the immunologic factors proposed for infertility (20% of all
causes of infertility) is presence of SA, ASAs in sera of infertile men
and women, seminal plasma, cervical mucus, and follicular fluids [1,2].
Rumke [3], Wilson [4]
were the first to report the presence of antisperm antibodies (ASAs) in
infertile men. Now ASAs are defined as immunoglobulines (Ig) of the
IgG, IgA and/ or IgM class that are located to various sites of the
spermatozoa (head, tail, midpiece or combination thereof) [2].
The incidence of sperm agglutination due to autoimmunity in infertile
couples is 9-36% in contrast to 0.9-4% in the fertile population. The
incidence of detection of ASAs in the fertile male is 8-21% and in the
female 6-23%. Immunological cause may contribute to 5-15% of the male
infertility factors [5].
It was reported that immunologic infertility is possible if more than
50% sperm are bound to IgG or IgA antibodies and it may be suspected if
more than 10% spermatozoa are antibody bound. An un-symptomatic immune
response to certain tissues of the reproductive system can cause
infertility [5,6].
Furthermore, presence of ASAs in the female
reproductive tract can prevent their motility through the female
reproductive tract or prevent the process of fertilization [2,7] and decrease the cleavage rate in patients with high titer of ASAs following IVF [8].
Finally, all these immunological infertility factors
that lead to the development of SA and ASAs among Yemeni infertile
patients are prevailing and are yet to be evaluated, thus enabling us to
take the necessary measures of prevention and treatment. On the other
side, SA and ASAs lab tests are still subjects of debate and there is a
lack of consensus on clinical consequences of ASAs. We hope our present
study will define the importance of SA and SSM screening in the process
of diagnosis of immunological infertility and their relationship with
infertility by involving large number of infertile patients with high
percentage of SA, and high ASAs in their semen and sera and long
duration of this study. Furthermore in all Yemeni labs (governmental and
private) the seminal fluid reports do not include percentage and types
of SA, percentage of SSM and ASAs tests as a routine test for diagnosis
of immunological infertility. All these problems give us strong impetus
to study them thoroughly. So, the present study is aimed to:
- Investigate the infertile patients with immunological infertility through the assessment of their results of semen analysis, SA, SSM and sperm-cervical interaction.
- The necessity of including fresh micro-slide SA and SSM lab technique as a routine clinical lab tests for diagnosis of immunological infertility.
Patient and Methods
Patients
Two hundred and eight infertile couples involved in
this study. Complete physical, medical, and infertility data were
documented and diagnosed as infertile cases with positive sperm
agglutination and sperm shaky head movement. Their sex and thyroid
hormonal profiles and prolactin were within the normal values. There was
no history of administration of glucocorticoids at least for 3 months
prior to participation in the present study and seminal fluid culture
and sensitivity was negative for pathogenic bacterial growth. They were
inspected for any history of testicular trauma, mumps, orchitis,
testicular torsions, varicocele, cryptorchidism, surgical intervention,
sterile seminal fluid infection. All husbands have positive anti-sperm
antibodies (ASA) in own sera and seminal fluid. The institutional review
board at Colleague of Medicine and Health Science, Sana’a University
approved the protocol, and couples gave written informed consent. All
wives were normally reproductive and fertile. According to the
percentage of agglutination, patients was divided into 2 groups
(Group-1<10% and group2>or =10%). According to age factor,
patients were divided into 3 groups. Group 1 less than 30, group 2:
31-40 and group 3 more than 40 years in age. All these groups were
compared to normal fertile men. The sperm agglutination and sperm shaky
head were the main factors. Intrauterine insemination was performed for
all couples.
Spermogram and its evaluation
Written informed consent was obtained from all
participants after recruitment. Semen samples were collected by
masturbation at the site of our center, after the men had been asked to
abstain from ejaculation for at least 48 hours before semen was
collected. All semen analyses were performed manually within one hour
after the sample was collected and included measurements of the volume
of the ejaculate and determinations of the sperm concentration and the
percentage of sperm motility, shaky head movement, agglutination and
morphology. Tow-three semen specimens were obtained from each man who
was involved in the present study. The number of days between the
specimen collections was from 25-42 days. The mean values for each semen
sample were calculated in studied by slide method. Semen fluid analyses
were performed in our external out-patient lab-according the guidelines
of the World Health Organization [9].
Sperm agglutination
Agglutination of spermatozoa means that motile
spermatozoa stick to each other – head to head agglutination, tail to
tailor in a mixed way, e. g. med-piece to tail. The adherence either of
immotile spermatozoa to each other or of motile spermatozoa to mucus
threads, cells other than spermatozoa, or debris is considered to be
nonspecific agglutination. The specimen was observed for sperm
agglutination by preparing a drop (50µL) of semen into a warm
microscopic slide covered by a cover slip. The presence of sperm
agglutination with shaky sperm head was suggestive of the existence of
an immunological cause of infertility. The extent of agglutination was
important. The presence of only a few groups of small numbers of
agglutinated spermatozoa was also recorded. Sperm agglutination and
interaction between spermatozoa were graded as:
+ (Sub-mild sperm agglutination)---------------<=10%
++ (Mild sperm agglutination)-------------------10-20%
+++ (Marked sperm agglutination)-------------21-40%
++++ (Very marked agglutination)------------->40%
For estimation of percentage of sperm agglutination the following formula is used:
Percentage of agglutinated sperm = No. of agglutinated sperms x 100
Total number of spermatozoa
Sperm shaky head movement: was determined by the same formula applied to the above mentioned for sperm agglutination.
Sperm-cervical mucus interaction
For fertilization to take place in -vivo, the sperm
must be able to get past the cervical mucus. The post coital test
assesses the ability of sperm to penetrate and progress through cervical
mucus. Cervical mucus is examined 2-3 hours after intercourse at the
time of expected ovulation. A presence of greater than 10-20
motile sperm per high power field is generally accepted as a normal
post coital test. Post coital testing is a bio-assay that provides
information concerning sexual function. Motility of the sperm, and the
sperm –mucus interaction. A positive results implies normal semen and
mucus. Poor results in an individual with normal semen parameters imply
either cervical abnormality or the presence of sperm antibodies.
Statistical Evaluation
Data were analyzes within built functions within the
Statistical Package for Social Science (SPSS UK Ltd, Chertey, Surrey,
United Kingdom). We used student’s t-test and multiple analysis of
variance (MANOVA) to determine the level of statistical significance
between the means and correlation test. Differences were considered
statically significant at P<=0.05.
Results
Two hundred and eight infertile couples were studied
in this research. No significant differences between the age and body
mass index in both groups, Table 1.
The duration of infertility was significant increased in group of
patients which their semen analysis recorded sperm agglutination more
than 10% (Table 1).
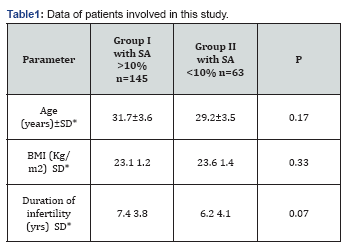
SD: Standard Deviation; BMI: Body Mass Index
The seminal fluid infection was recorded as the
higher percentage of causes of infertility in patients group-I in
compared to patients in group-II (47.62 and 41.38%, P 0.03,
respectively). The idiopathic causes of immunological infertility still
in the second place, (Table 2).

According to the age factor, the Figure 1
demonstrates that sperm agglutination was noted significantly (P=0.002)
higher in age group 2 (30-40 years) compared to age group 1 and 3.
Percentage of sperm shaky head movement was significantly, P=0.03, in
the age group 3 compared to age group 2 and 1, (Figure 1).

The results of sperm cervical interaction are demonstrated in Figure 2.
The percentage of motility of sperm recovery was significantly better
in age group 2 compared to age groups 1 and 3. At the same time the
heist sperm concentration recovery as well as sperm agglutination were
significantly (p=0.02) higher in age group 2. While percentage of
recovery sperm shaky head movement was recorded in age group 3, Figure 2, P=0.004, compared to age group 1 and 2.

Discussion
Two hundred and eight infertile couples were involved
in this study to find the common causes of immunological infertility.
It was found out that more than 60% of patients involved in the present
study suffered from sterile seminal fluid infection who have a positive
concentration of ASA in own sera. These results were in good agreement
with that reported by Rusz et al. [10].
Presence of sterile seminal fluid infection (i.e no
bacterial growth after culturing of ejaculate) or previous orchitis lead
to damage of blood-testis barrier (BTB). Physiologically, the BTB is a
tight junction between Sertoli cells and appears to play a major role in
keeping the developing spermatozoa and immune system separate. It
prevents those testicular cells expressing “foreign” antigens from
coming into contact with lymphoid tissue and immunocompetent cells from
entering the seminiferous tubules [11]. However, the BTB is commonly breached by physiological leakage of normally sequestered sperm antigens.
When the BTB were damaged due to infection these
antigens come into contact with immunocompetent cells, ASA formation
occurs and lead to formation of auto-immunity against own sperms [12]. Bronson [13]
reported that the active local immunoregulatory mechanisms start being
operative within the testes. Autoimmunity to sperm may occur because
sperm cells antigens are first expressed during sexual maturation [14], long after the prenatal period when immunological self-tolerance is induced [7,15,16].
Generally, every breakdown of blood-testis barrier
and protective immunomodulatory mechanisms or hormonal immune response
such as ASA formation can be induced primarily during infectious and
noninfectious inflammations lead to immunoinfertility, or by obstruction
of testicular efferent duct- obstructive azoospermia [12].
The ASAs were also induced after accidental and /or surgical injury of
testicles, exposure to very low temperature or cryptorchidism [17,18].
Subsequently, infertility can result from antibodies directly binding
the sperm, or from spermatogenesis due to orchitis. A similar phenomenon
occurs in vasectomized laboratory rodents and man [17].
Most affected individuals developed epididymal sperm
granulomas and testicular degeneration associated with the formation of
ASAs. Mechanisms that can provide the autoimmunity and ASA production
are micro-environmental acceleration of T-helper-type-1 (Th1) of
immunity, enhanced secretion of pro-inflammatory cytokines like IL-1,
reduced secretion of anti-inflammatory cytokines like IL-10 and TGF-_,
up-regulation of MHC and co-stimulatory molecules expression and
down-regulation of immune cells apoptotic mechanism [17].
Finally, the presence of sperm agglutination >10% of viable sperms
without bacterial seminal fluid infection and high concentration of
serum ASAs reacting with antigens on the sperm are considered typical
and specific immunological infertility [19].
The indication for ASAs testing in these infertile
patients was abnormal semen parameters which include high percentage of
SA, SSM, poor sperm motility and poor sperm mucous interaction tests
(postcoital test). All these tests were strongly and significantly
higher in group-I when compared to group-II. These sperm parameters were
also positively correlated significantly with high concentration of
their own sera ASAs and poor sperm mucous interaction tests of their
wives. In the last decade there are a lot of reports on human ASAs and
interference of some of them with reproductive physiology. It is
supposed that sterile seminal fluid infection and high percentage of SA
associating with high concentration of ASAs and binding to sperm surface
which inhibit sperm function parameters and fertilization and the
presence of circulating ASAs in uterine cervix of women have been implicated as a contributing factor to immunological infertility [6].
In these studies, the incidence of subsequent pregnancy in infertile
couples was absent if one or both partners had ASAs in serum [20] or in genital tract secretions [21].
According to other reports, the prevalence of ASA positive cases in men
and women with unexplained infertility was significantly more than
cases with explained infertility. This certifies that ASAs affect
fertility [22] and this relationship had been confirmed in our present work.
Regarding the aforementioned studies, the concept of
ASAs in fertilization is based on their presence in serum and different
secretions of the human reproductive tract [23]. Although some studies have pointed to the higher prevalence of ASAs in infertile patients [1].
Recently, it was successfully recommended the using of phage display
technology to obtain antisperm scFv antibodies of defined antigen
specificity. These antibodies will find clinical applications in the
development of novel immunocontraceptives, and specific diagnostic for
immunological infertility [24].
The positive correlations between percentages of
sperm agglutination as well as shaky head movement and ASAs titers
indicated that sperm agglutination and sperm shaky head movement should
be used as a good and simple lab tests indicators for the presence of
ASAs in the own sera and seminal plasma as well as good indicator for
diagnosis of immunological infertility. Ability to diagnose carefully
will lead to right way of treatment. Finally, using of these lab test
techniques is useful, answerable and acceptable methods for diagnosis of
immunological infertility [25].
Our study does not agree with the result presented by Karimi et al. [2] for the following reasons:
- The group of patients involved in their study had unexplained infertility and such group of patients have to be infertile with unknown causes.
- The researchers did not present any data about their spermogram including sperm agglutination, sperm shaky head movement, etc. It is our belief that such groups of unexplained infertility are a matter involving divine powers and keeping them unexplained infertile. Such group should not be subject to experimentation. Probably, for these reason the authors did not find any significant differences. That is true because it is unexplained infertility. It is our belief that the cases of such group (unexplained infertility) are unexplainable and fall in the domain of divinity.
Conclusion and Recommendation
We concluded that:
- 60% of causes of immunological infertility mainly associated with sterile seminal fluid infection.
- We emphasized on the importance of percentage of sperm agglutination and sperm shaky head movement should be associated with high titer of ASAs in their sera and seminal plasma.
- The recovery of sperm –cervical We recommend the use of these so simple useful, accessible, and reliable lab tests as a routine investigation for diagnosis of high titer of ASAs as well as immunological infertility and should be considered seriously.
- We advise that such tests should be involved in medical reports regarding infertility and expect that the authorities concerned in the ministry of health will put into effect all our suggestions and help to diagnose of immunological infertility.
Acknowledgement
First of all, authors would like to thank all workers
in Allow IVF Center, Sana’a Yemen for support and permission to use
their data for publication of this work. At the same time authors would
like to thank the Faculty of Medicine and Health Sciences for getting
ethical approval for this work.
Funding
For analysis and publication. Research Initiative Grant Scheme (RIGS-15-083-0083).
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/
To read more......Fulltext in Gynecology
and Women’s Health in Juniper Publishers




Comments
Post a Comment