Juniper Publishers: Laparoscopic Surgery of Massive Ovarian Edema: A Case Report and Literature Review
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Yuji Tanaka*
Massive ovarian edema (MOE) is a rare benign clinical
entity that can be confused with neoplastic ovarian tumor. Usually,
ovarian torsion develops secondary to an ovarian tumor, but at times, it
might develop even in a normal ovary. Most MOE occurs because of
intermittent torsion of the normal ovary and compromised venous or
lymphatic drainage, which subsequently involve the arteries. The major
symptoms of MOE are abdominal pain, due to torsion of the stem. Since it
is not a neoplastic disease, a therapy that preserves fertility should
be the principle of treatment. We present here, our case along with a
literature review on the subject. A 9-year-old girl was admitted in our
hospital with abdominal pain and was diagnosed with MOE based on
ultrasonography and Magnetic Resonance Imaging findings. After the first
onset, conservative therapy with analgesics was administered for about 7
months during repeat exacerbations. A second episode of severe
abdominal pain occurred after 7 months. Although ovarian blood flow was
preserved on imaging investigations, laparoscopic surgery was performed
due to increasing pain. Untwisting and wedge resection of the ovary and
ovarian fixation was performed. Clinical follow-up at 5 months using
ultrasonography examination revealed no recurrence of the torsion. If
the ovarian blood flow is maintained as in this case, conservative
treatment is possible, but surgical therapy is considered if there is a
worsening of symptoms such as pain or absence of ovarian blood flow.
Laparoscopic surgery for untwisting the torsion is initially
recommended. Wedge resection of the ovary should be considered. There
are pros and cons for ovarian fixation, but it should be enforced in
cases where there is a concern about revolving easily.
Keywords: Massive ovarian edema; Ovarian torsion; Laparoscopic surgeryAbbreviations: MOE: Massive Ovarian Edema; CT: Computed Tomography; MRI: Magnetic Resonance Image
Introduction
Massive ovarian edema (MOE) is a rare benign clinical
entity that could be confused with neoplastic ovarian tumor. The
average age of patients with MOE is about 20years [1,2];
hence, preserving the ovary should be the goal of therapy for these
patients, in order to preserve hormonal function and fertility. We
report a case where we preserved the ovaries and prevented recurrence
through conservative treatment and laparoscopic surgery. We also present
a literature review for this condition.
Case Presentation
A female patient aged 9 years was admitted with a
history of right abdominal pain of 3days duration. Ultrasonography
revealed a partly solid and cystic mass with thick contents and
measuring 4cm, arising from the right ovary. The mass appeared to be
freely mobile, with a smooth surface. Ovarian blood flow was preserved.
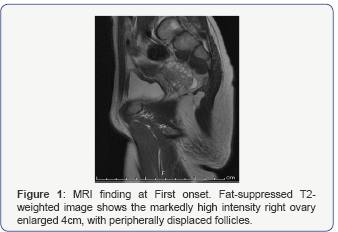
Computed Tomography (CT) revealed similar findings. T2-weighted
abdominal magnetic resonance images (MRI) showed asymmetric ovarian
enlargement in a teardrop configuration, hyper intense peripherally
displaced follicles, and twisting of the vascular pedicle between the
enlarged ovary and uterus (Figure 1).
On laboratory investigations, the hormonal levels were in the normal
range as expected in a female before menarche. Tumor markers were under
the limits. A diagnosis of MOE was made. Conservative treatment with
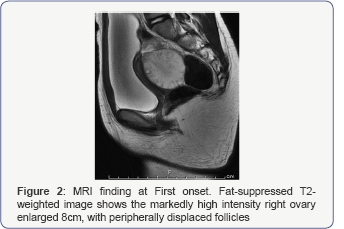
analgesics was success. A second episode of severe abdominal pain
occurred 7 months later. Ultrasonography and MRI showed that the right
ovary was enlarged to 8cm (Figure 2).
Conservative treatment with analgesics and defecation and bladder
catheterization was administered for 3days. Although ultrasonography
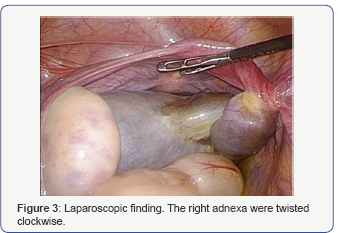
showed that the ovarian blood flow was preserved; laparoscopic surgery
was performed due to severe, increasing pain. On laparoscopy, the right
ovary was enlarged, edematous (8cm), rotated by 540 degrees, and
displaced to the posterior side of the broad ligament (Figure 3).
The surface of the right ovary was reddish brown. The left ovary was
slightly enlarged (4cm). The uterus appeared normal in shape and size.
After untwisting the ovarian ligament and the fallopian tube, wedge
resection of the right ovarian cysts was performed.
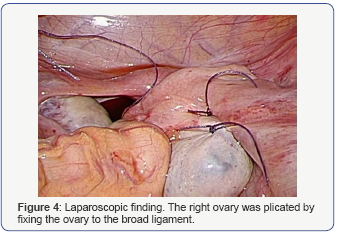
After untwisting, the color of the ovary promptly returned to white and
pink. The right ovary was fixing the ovary to the broad ligament, as the
ligament was extended and the risk of re-twisting was high (Figure 4).
The postoperative period was uneventful. On the fifth postoperative
day, ultrasonography revealed shrinkage of the right ovarian diameter to
6cm. She was discharged on the sixth postoperative day.
Histopathological findings showed noneoplastic change, but presence of
MOE. At 5 months post-surgery, no recurrence was seen, and the ovaries
we real most normal size.
Discussion
MOE was first described by Kalstone et al. [3], and is defined by WHO Formation of a tumour-like enlargement of one or both ovaries by oedema fluid [4]. MOE patients are between 6 and 33 years of age, and the average age is 21 years [1,2,4].
There are two types of MOE: primary MOE occurs when
the ovary is not diseased but there is torsion or twisting of the
ovarian pedicle to the extent that it interferes with the venous and
lymphatic drainage leading to edema, but does not affect the arterial
blood flow. The major symptoms of primary MOE are acute or chronic pain,
and the duration of pain depends on the character of the torsion [5]. The condition frequently occurs on the right side; accounting for about 75% of cases [6],
probably due to higher pressure in the right ovarian vein caused by the
distinct anatomy of venous drainage from the right ovary [7]. Secondary MOE occurs in a diseased ovary, such as ovarian tumor [8-12] and malignant tumor [13-15], or in patients on hormonal therapy for ovulation induction [16]. Various theories have been postulated about the mechanism of onset of secondary MOE [17]; however, there is no established mechanism yet. Of all MOE cases, 85% are primary, and 15% are secondary [5].
In the past, pre-operative diagnosis of MOE was
difficult, and most cases were diagnosed based on the postoperative
pathological findings. Many cases were over-treated due to the confusion
with ovarian malignant tumors. In a series by Praveen et al. [5]
82% of the cases were subjected to salpingo-oophorectomy and 7% to
total hysterectomy and bilateral oophorectomy; only 11% patients under
went fertility-preserving surgery [5].
However, in the current times, MRI and ultrasonography enable a precise
preoperative diagnosis. The typical findings on MRI and ultrasonography
are multiple cysts at the peripheral cortex of an enlarged ovary. The
image findings depend on histological characteristics [18-21].
Histological, multiple ovarian follicles at the peripheral cortex and
edematous ovarian stroma are seen, and the ovarian architecture is
preserved [22].
An important aspect of treating young women with MOE
is the preservation of fertility and preventing multiple surgeries.
There are two possible approaches to MOE: conservation therapy or surgical treatment. Guvenal et al. [23]
reported that MOE could be managed conservatively, if ovarian blood
flow is maintained on ultrasonography, as in our case, conservative
treatment should be the first choice of therapy. Conservative treatment
of MOE includes administration of analgesics, indwelling catheterization
of the bladder and/or injection of saline into the bladder, aiding
defecation, and waiting for a natural untwisting of the ovarian torsion.
Surgical therapy is necessary if there is a worsening of symptoms such
as pain or absence of ovarian blood flow. Laparoscopic surgery is
recommended, since it is less invasive than laparotomy, and offers both
diagnostic and therapeutic advantages [24-28].
Laparoscopic untwisting of the ovarian torsion is the basic surgery for
primary MOE. However, the optimal surgical procedure following
untwisting of the ovarian torsion is still unknown. There are two
surgical options, wedge resection of massive ovary or ovarian fixation.
Prevention of recurrence of the torsion is expected due to volume
reduction in wedge resection [25,26,28],
but formation of adhesions is a cause for concern. If the diagnosis of
MOE cannot be confirmed on preoperative investigations, or a malignant
tumor is suspected, histological analysis of the frozen sample obtained
during wedge resection of the ovary can lead to a confirmatory diagnosis
[27].
Some authors have recommended fixation of the ovary to the posterior
aspect of the uterus or broad ligament or round ligament, for prevention
of torsion recurrence [28-30]. Some other authors do not recommend ovarian fixation surgery as this might reduce the blood flow and function of the ovary [31], and might not prevent recurrence. The type of surgical technique to be employed needs to be individualized for each case.
Acknowledgment
The authors would like to thank Dr. Michio Yamasaki and Katsuji Imoto for their help with radiological considerations.
Conflict of Interest
The authors report no declarations of interest.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment