Juniper Publishers: Placental Accretism before 20 Weeks of Gestational Age
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Ricardo Illia*
Introduction
Defined as placental accretism, is the abnormal partial or total adherence of the placenta to the underlying uterine surface [1]. It is little common to find this anomaly in the first half of pregnancy.
In more advanced pregnancies, Miller et al. [2]
report that the placental accretism occurred in 9.3% of patients with
placenta previa versus 0.004% in patients without previous placenta (RR
2.065, P< 0.0001). Between patients with placenta previa, accretism
risk was increased in patients over 35 years and with a history of
previous c-sections. Is interesting to take in consideration the
reflections of Chau et al about the cytoquines role in the placental
advance into the myometrium.
In terms of the accretism in the first half of the pregnancy, the posted information is scarce and only on isolated cases.
Wheeler et al. [3] report a case diagnosed by ultrasound at 18 week´s of gestation, that ended in a total hysterectomy before fetal viability.
Arredondo et al. [1]
reported a case of accretism in first trimester requiring total
hysterectomy for resolution at this stage of pregnancy. This patient
presented as risk factor associated with a history of three uterine
curettages to end early pregnancies.
Bernal & cols [4]
in a patient of 19 weeks of gestational age with signs of acute
abdomen, performed a laparotomy, finding an uterine rupture with
placental percretismo requiring total hysterectomy.
Kinoshita et al. [5]
report a case of placental percretism which arose as an acute abdomen
at 25 week´s of gestational age, which required a total hysterectomy
with diagnostic presumption through pathology confirmation for this
treatment. This patient had no history neither previous pregnancies nor
operations in the womb. Mueller et al. [6]
reported a case of similar developments at 18 weeks pregnancy but the
attributable cause of spontaneous uterine rupture was an adenomyosis.
Monks et al. [7]
reported a case of cervical pregnancy with associated placental
percretism, both diagnoses were performed successfully by
ultrasonography and analyzed conservative or aggressive therapeutic
possibilities according to the general condition of the patient.
Slomko et al. [8]
presented a case of placental percretism during abdominal caesarean
section, and pose considered therapeutic alternative to resection of the
myometrium committed to the further metroplastia.
Durand Reville et al. [9]
report that the diagnosis of placental accretism and percretism can be
done by ultrasound B-mode and Doppler color. The extension of placenta
very vascularized to the myometrium, complex placenta-subplacenta
abnormal and flow vascular through the myometrium suggest the diagnosis.
In the present times, is common to add magnetic [10].
resonance to help to make the diagnosis of accretism, but some authors said that is not neccesary because ultrasound is enough [11-13].
As mentioned at the beginning of the review,
information on anomalies of placentation in early stages of pregnancy is
rare and isolated, presenting a history of risk caesarean section and
uterine curettages or in some case even without a history of risk. Also
we have to take in consideration the gynecological procedures into the
uterus such as hysteroscopy and myiomectomies.
Then we will present four cases of accretism or placental percretism in pregnancies of less than 20 weeks of gestational age.
Case 1
30 year-old patient who consults with menstrual delay
of 6 weeks, positive gonadotrophin, with a history of two previous
c-sections. It begins with little genital bleeding so is medicated with
progesterone and rest. The bleeding does not generate any associated
pain, motive by wich it was performed an ultrasound that shows
gestational sac normoimplanted without embryo. A new
ultrasound reports egg without embryo so it was decided expectant
management given the reduced size of the gestational sac (30mm). The
patient will not cameto office for about 6 weeks, period after which
consultation again referring absence of bleeding but either not had
menses.
The gynecological examination presents soft uterus,
increased in size as 3 months of pregnancy. Evacuator curettage is
scheduled. During the surgical act, the feeling on the curette is of
consistency soft and soon after starting curettage the uterus started to
bleed with a metrorrhagia each time more intense, that not reversed
with oxytocic. This picture is of such intensity that despite blood
transfusions undertaken the general condition of the patient was
impaired. It was decided to carry out exploratory laparotomy and
observed uterus in barrel with bluish appearance, soft consistency. A
total hysterectomy is performed and the patient evolved favorably. The
pathology report, reveals placental accretism.
Case 2
43 year-old patient who consults with 7 week´s
pregnancy. Obstetric history has two previous c-sections (the last 18
years ago). Started with threatened abortion and at consultation
presents abortion in progress with removal of remains for external
cervical OS. Described evacuator curettage which is initially carried
out without problems, but a bit of starting the procedure occurs
unenforceable metrorrhagia of red blood, to then see absence of ability
to coagulate. In the absence of systemic manifestations of coagulopathy
and the profuse of metrorrhagia with severe compromise of the general
condition of the patient it was decided to practice a total hysterectomy
with resolution picture and recovery of the general condition of the
patient after two days of hospitalization in intensive care unit. The
pathology of the surgical specimen reported placenta accreta.
Case 3
Patient 43-year-old with a history of two previous
c-sections, the last 9 years ago. With pregnancy confirmed by beta HCG
(60 U) 7 weeks, is presented to the consultation with abundant bleeding
of red blood. Ultrasound evaluation reports uterus 106mmx36mmx49mm with
deformation before the istmic-body showing ecoestructural alteration
with solid area and more liquid which altogether measure 48 x 17 x 34
mm. Image is under the previous caesarean section scar and at that level
the echo endometrium-cavitary is identified. In addition liquid area
shows a strong wall image of 9mm.
Faced with this situation, with the firm suspected of
trophoblast invading the myometrium and the risk of producing a
solution of continuity if we perform a curettage, the Department at
debate considered convenient to try to inactivate the trophoblast
administrating methotrexate, which was administered at a dose of 50
mg/kg. After 24 hours of drug administration the patient presents to the
ultrasound examination a 42x21x28xmm with 10 mm embryo sac. At 48hr the
ultrasound report was similar and the patient receives the transient
discharge from hospital. After 48 hours of discharge, the ultrasound
image shows sac with multiple internal echoes and beta HCG value was 30
u. with patient asymptomatic. The last ultrasound showed an image of
24x20x21mm on the scar with beta HCG negative. After 30 days, the
patient is asymptomatic with normal gynecologic ultrasound and beta HCG
still negative.
Case 4
Patient of 38 years with a history of a previous
c-section and 3 uterine curettages to evacuate stopped pregnancies. At
booking, the patient continued with persistent and continuous bleeding
from two months ago, when it was performed a curettage because stopped
pregnancy. It is admitted in the obstetrics service for study and
evaluation. The beta in blood was low positive (300mu/ml). Study
ultrasound, in principle showed images compatible with trophoblastic
disease. He was tried in principle the uterine evacuation using vaginal
and oral misoprostol without success, so it was decided to perform an
intrauterine aspiration for evacuation of its content.
Under general anesthesia the procedure begins, and
immediately started, the patient begins with intense bleeding that does
not respond neither to drugs to contract the uterus and stop bleeding
nor curettage of the uterine cavity. With hemodynamically compromised
patient, decides the placement of a of Bakri balloon, stopping bleeding
with filling with 500cc saline. Because the bleeding, maneuvers were
suspended until improvement of the general condition of the patient who
was sent to intensive care unit for recovery. To the 24hs of evolution,
with the patient hemodynamically stable, was observed by ultrasound and
magnetic resonance that the balloon was free in the pelvis, outside of
the uterus. This allows to deduce that hemostasis was accomplished by
compression of the uterus against the sacrum when the balloon was
filled. In front of this situation, it was decided an exploratory
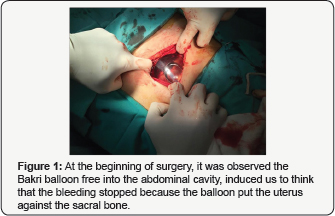
laparotomy. Open peritoneum, hemoperitoneum and the balloon in cavity (Figure 1)
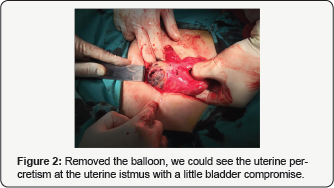
is observed. Withdraws it, noting the uterus with clear signs of
trophoblastic invasion. We decided to make a total hysterectomy to
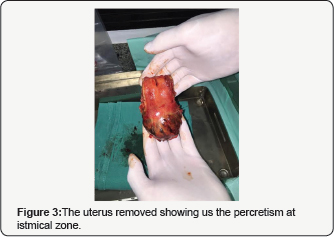
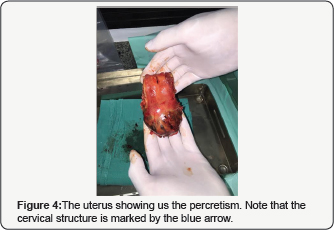
resolve the problem that was accomplished with success (Figure 2). Hysterectomy piece clearly showed a placental percretism with mild commitment of the bladder which was dissected and liberated to be able to remove the uterus (Figure 3). The patient was in perfect state and she was discharged 96hrs of postoperative evolution (Figure 4).
Discussion
Apparently we have a very rare entity as revealed by
the literature search, but able to act with an unusual gravity still in
early stages of gestation, with pictures of profuse bleeding which
seriously compromise the health of the patient and whose most frequent
solution is thetotal hysterectomy. Mostly these patients presented the
factors of risk set forth by Miller & cols [2]: maternal age over 35 years and history of Caesarean sections and curettages in the past.
Up to the present time, these factors were taken into
account as at risk for placental accretism in more mature pregnancies,
since the accretism is increasingly common in direct relation to the
increase in the incidence of caesarean sections.
But the cases presented, together with the cases presented in the literature [1-8]
describes a serious clinical picture, low frequency but high severity,
in less than 20 weeks pregnancy. Some professionals adopt behaviors
expectantly before diagnoses of detained pregnancies or anembryonic eggs
on the idea of obtaining full or partial spontaneous evacuation to
avoid traumatic cervical dilatation with Hegar dilators which could
produce a subsequent cervical incompetence. Of agreement to these
observations, this behavior in the event that the patient as a history
of caesarean or have 35 or more years, you can keep this way of
following of the patient, but with close ultrasound control to allow the
opportunity to diagnose a possible placental accretism.
If the patient is with profuse bleeding, treatment
generally is total hysterectomy since bleeding is by direct vascular
lesion produced by the trophoblast in its myometrial invasion. In the
case of a placental accretism is suspected, treatment with methotrexate
is a valid alternative to try to avoid a surgical treatment at first
instance, but in the case of heavy bleeding, the only treatment is the
hysterectomy, because is weird that embolization treatments should be
successful in front of such amount of bleeding. The administration of
one or more series of methotrexate dose of 50mg/kg of weight via
paraenteral with an ultrasound monitoring and quantification of beta HCG
is presented as a possibility to avoid radical surgical treatments in
pathology from the first half of pregnancy.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment