Juniper Publishers: Common iliac Artery Pseudo Aneurysm as a Complication of Diagnostic Laparoscopy
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Purohit P
Keywords
Keywords: Veress needle; Aneurysm; Laparoscopy; Vascular injury; StentIntroduction
In UK, a quarter of a million women undergo laparoscopic surgery each year most of which are without any serious complications [1].
Vascular injury, albeit rare, is a major life-threatening complication
of laparoscopy and it is difficult to determine the exact incidence due
to its rarity and possible under-reporting. The published rates vary
between 0.1 to 1.05/1000 cases with maximum risk reported during e the
phase of entry i.e from insertion of optical port until visualisation of
the intrabdominal contents [2,3].
We report a case of Visceral Artery pseudo aneurysm
(VAP) of the Right Common Iliac secondary due to Veress needle insertion
during a gynaecological surgery.
Case Report
A 29 year female underwent diagnostic laparoscopy to
manage uterine perforation during a hysteroscopic surgery. The
laparoscopy was carried out by routine closed entry technique with
single passage of Veress needle for pneumoperitoneum followed by 10mm
intra-umbilical port and 5mm lateral accessory port. A small uterine
fundal perforation was sutured with 2-0 Vicryl. The total procedure time
was 90 minutes. The blood loss during the procedure was minimal.
The patient presented with severe abdominal pain and
transient hypotension during the post-operative period. Her observations
settled with fluid resuscitation and she was kept overnight for pain
control. An urgent post-operative Hb showed a drop in Hb (pre-op=139g/L,
post-op=88g/L). On examination, abdomen was soft with no guarding or
rigidity. Due to persistent post-operative pain and disproportionate
fall in Hb, an urgent CT scan was arranged.
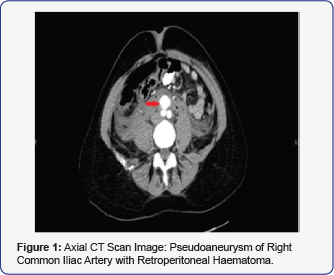
CT showed a large retro peritoneal haematoma
extending from renal veins up to the pelvis with pseudo aneurysm of the
Right Common Iliac Artery measuring 21x27x17mm just below the aortic
bifurcation (Figure 1).
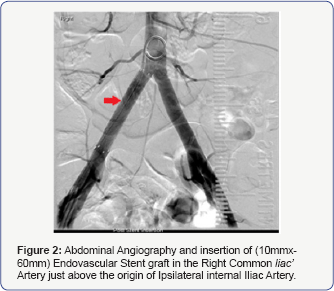
Retrograde puncture of the ipsilateral common femoral artery was
performed under ultrasound guidance followed by insertion of a 7 French
sheath. A pigtail catheter was sited into the distal aorta, allowing for
angiographic identification of the pseudoaneurysm origin. A 10 mm
diameter balloon-mounted Advantage V12 covered stent (Atrium Medical,
USA) was then deployed within the common iliac artery, excluding flow
into the aneurysmal sac. A percutaneous 10mmx60mm Endovascular Stent
graft was inserted in the Right Common Iliac Artery pseudo aneurysm (Figure 2).
Post stent angiography demonstrated satisfactory flow within the
vessel, with no filling of the pseudoaneurysm. The access site was
sealed with deployment of an Angioseal collagen plug closure device.
This procedure was uneventful. The patient was put on dual anti-platelet
therapy (Aspirin+Clopidogrel) and LMW heparin.
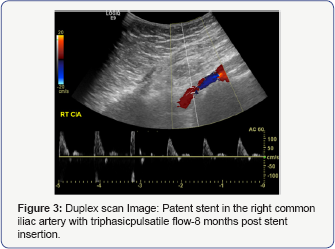
She was transfused 2 units of blood and then
discharged a week later after her original procedure. She was jointly
followed up by the gynaecology and vascular team. A duplex scan done 8
months post stenting showed a well embedded and patent stent in the
right common iliac artery with triphasic pulsatile flow and no stenosis.
No pseudo aneurysm was seen during this examination (Figure 3).
Discussion
Visceral artery psuedoaneurysms (VAP) can develop as a
result of blunt or penetrating trauma, inflammation, infection,
vasculitis, and iatrogenic trauma secondary to surgical, endoscopic, and
radiologic procedures. In traumatic VAPs, the pathologic feature is
deficiency of the arterial media with loss and/or fragmentation of the
connective tissue and smooth muscle. The VAP in this case was attributed
to the blind technique of Veress needle insertion. Alternative to the
blind Veress needle insertion technique is the open Hasson’s technique.
However, based on the available evidence there is no consensus in
regards to the superiority of one technique over the other [4].
The open technique is associated higher bowel injuries as compared to
the closed technique. However, quality of evidence in this regards is
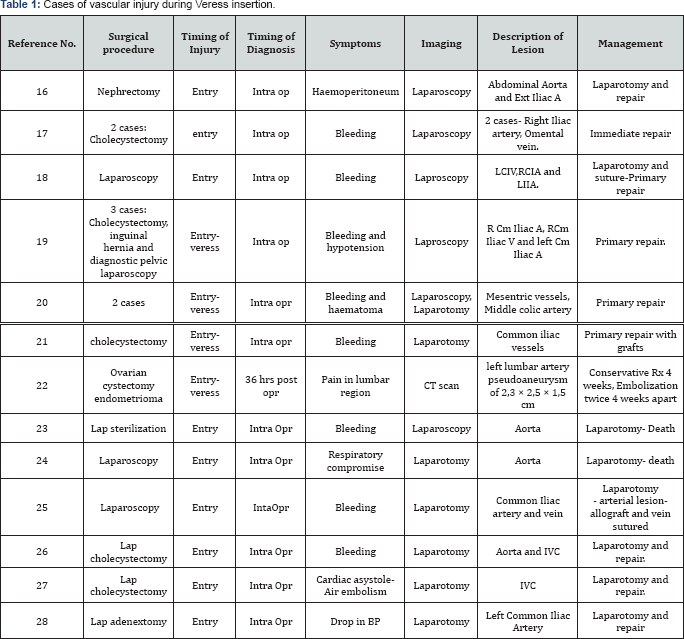
poor [5]. The risk of vessel damage was so low in both groups that no statistical difference was observed (Table 1).
This procedure was performed by an experienced laparoscopic surgeon. As per the analysis done by Schäfer et al. [6]
85% of the major vascular injuries caused either by experienced
surgeons (those who had performed between 51 and 100 procedures) or very
experienced surgeons (over 100 procedures performed). Thus, it is
essential that the position of the needle tip after insertion be
determined as accurately as possible and with great care.
Complications of VAPs can be life threating which
include early rupture, compression of adjacent structures,
thromboembolism and a higher frequency of aneurysm infection. Lack of an
intact vessel wall leads to continued enlargement and subsequent
rupture in nearly all cases of visceral pseudo aneurysms necessitating
prompt and accurate treatment. In this particular case, post-operative
pain and drop in haemoglobin level were the symptoms which prompted
further investigations to diagnose the VAP. The mainstay for diagnosis
of VAPs is the conventional angiography but is an invasive procedure and
non-invasive diagnostic modalities like CT scan, MRI both combined with
Angiography and colour Doppler Ultrasound study should be included in
the initial work-up if possible [7]. In our case, the VAP was diagnosed on a contrast CT scan.
Another aspect highlighted through this case is the
novel approach towards management of arterial aneurysms. Traditionally,
internal iliac aneurysms have been repaired by surgical interposition of
graft particularly in aneurysms >40mm to prevent rupture [8,9].
This approach is challenging due to the difficult dissection and
surgical approach into the pelvis with high risk of visceral,
genitourinary and pelvic venous injury with carries a significant
morbidity and mortality of up to 10% [9].
With the advancement of endovascular techniques,
effective alternative is now available. Particularly in our case as the
aneurysm was close to the aortic bifurcation and minimally invasive
repair played an important role. The technique of endovascular repair of
a subclavian artery penetrating injury was first described in 1996 [10]. Similarly, Nyman et al. [11]
presented three cases of iatrogenic iliac artery perforations treated
by endovascular stent-grafting in 1999. There have been multiple
subsequent reviews and case reports of endovascular techniques for
arterial injuries throughout the body [12-14].
The mainstay of therapy is based on the use of
stent-grafts. First developed for treating aneurysms, stent-grafts
consist of a tubular metal scaffold covered with PTFE to create an
artificial lumen through which blood can be diverted. The benefit of
stent-grafts is that they can be packaged tightly within a small
diameter delivery device and inserted endoluminally through an arterial
puncture. They can be expanded in-situ, either by balloon inflation or
self-expansion, the latter of which relies on the shape memory
properties of the metal alloy Nitinol. With regards to focal penetrating
arterial injury to a relatively large vessel such at the common iliac,
stent-graft deployment can seal the point of haemorrhage without the
need for open surgical repair, significantly reducing the morbidity and
mortality associated with emergent laparotomy [15].
We would also like to stress here the need for
appropriate counselling and consenting of all women before laparoscopic
procedures. Women must be informed of the risks and potential
complications associated with laparoscopy.
Conclusion
VAPs although life threating are extremely rare. All
laparoscopic surgeons should be aware of the possibility of this
complication which can happen even in the most experienced hands. High
index of suspicion, early diagnosis and prompt treatment is the key
towards minimizing the morbidity and mortality associated with these
complications. This also depends on a great extent to the local
availability of imaging modalities and interventional radiology
services.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment