Juniper Publishers: Frailty Assesment and Risk of Osteoporotic Fracture in Women from a Case
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Miguel Ángel Acosta-Benito*
Abstract
Around 50 percent of the elderly women will present
an osteoporotic fracture. These fractures are related to the presence of
frailty syndrome, which appears linked to age with a prevalence of
10-25% in the same age group. The association between these two entities
shows the importance of a different method for evaluating of the risk
of fracture in the elderly women, incorporating the syndrome as a risk
factor that must be taken into account. Frailty, on the other hand, is a
good indicator to evaluate the effectiveness of the different
interventions related to osteoporosis.
Keywords: Frailty; Osteoporosis; Women; Risk of fractureAbbreviations: SPPB: Short Physical Performance Battery Test; BMI: Body Mass Index
Introduction
Frailty is a geriatric syndrome related to a decrease
in the functional reserve of the different physiologic systems. When an
aggression occurs, the patient loses her capacity to balance the
damage, resulting in an alteration of the homeostasis and secondary
negative health events [1].
The appearance of a hip fracture or other
(osteoporotic ones) in older women is a health event that is associated
with increased mortality and morbidity, as well as dependency. For frail
women it also implies acceleration in the evolution of frailty syndrome
due to its consequences: immobility, increase of infections,
sedentarism [2].
Osteoporotic fractures are more common in women, what makes it
especially important to apply preventive strategies and identify
indicators that allow a correct evaluation of treatments and
interventions on them, as functional capacity and frailty have become
more important than health events as a measure of quality of life and
prognosis in the elderly [3].
It is therefore important to be able to identify
frail women who have greater risk of hip fracture and other osteoporotic
fractures, as they clearly worsen their prognosis [4].
Through the presentation of a case, principal applications of frailty
identification related to risk of fracture will be described, as well as
the controversy and problems found in research in this field.
Case Report
The case of a 78-year-old patient, who in the last
three years unintentionally lost 8kg is presented. In her personal
history, she has arterial hypertension, obesity, diabetes mellitus,
grade IIIb renal insufficiency and intermittent asthma. She is not able
to climb 20 steps without stopping.
In the physical examination, an abdominal perimeter
of 120cm, with a BMI of 33, is highlighted. She has never received
corticosteroid therapy for long periods of time, has not had previous
fractures, does not smoke and has no other risk factor for osteoporosis.
The patient, in addition to the described
comorbidities, has frailty syndrome according to the FRAIL scale and
phenotype. An interdisciplinary handling of the case is established,
involving medical, nursing and physiotherapy professionals. In spite of
the efforts, the patient does not perform the prescribed exercises and
maintains an irregular feeding, so that her BMI increases to 36.
Two years after, the patient presents lower strength,
aerobic endurance and flexibility, worsening the score obtained in the
Short SPPB from 15 to 9 points.
At the age of 80, without any
special trauma or fall, she has a spiral left hip fracture, which is
surgically treated. Due to the characteristics of the fracture, bone
densitometry is performed with a T Score of -2.9 in the right hip and
-3.8 in the lumbar vertebrae. Antiresorptive treatment is started as she
is diagnosed of osteoporosis.
Taking advantage of the disposition of the patient in
coping with the rehabilitation of the fracture, it is possible to
establish life changes in terms of food and exercise, with weight loss
and increase of muscle mass against fat tissue, observed through
impedanciometry and by the SPPB scale.
Discussion
Frailty is a dynamic condition that refers to a
greater vulnerability secondary to the physiological changes typical of
aging and influenced by the patient’s life conditions and diseases. It
is directly related to age, and appears in more than 10% of people over
65 years, and in more than 25% of those over 85 [5].
Frailty syndrome affects women preferentially, not only in terms of
relative prevalence but also with a longer duration of the disease.
African-American women have higher rates of frailty [6].
Osteoporosis, defined as a reduction of bone mass
with altered bone microarchitecture, is usually diagnosed with the aid
of a densitometry (when bone density is less than 2.5 standard
deviations from that of a young, healthy woman), or after the appearance
of a frailty fracture. Due to population aging, it is estimated that
between 40 and 50% of women will present at the time of their life an
osteoporotic fracture [7].
It has been shown that the more frail a patient is,
the greater the risk of an osteoporosis-related fracture has, so
detection of frailty syndrome can help in the management of osteoporosis
in older women [8].
There is a relationship between the presence of
osteoporosis and sarcopenia, and between the last and frailty syndrome.
Locquet et al report that muscular mass and strength are lower in women
with osteoporosis. They analysed grip strength measurements, Dual-Energy
X-Ray Absorptiometry and physical performance by the SPPB [9]. Sarcopenia is related to body composition, with higher proportion of fat, as in the patient showed.
The large number of tools proposed to measure frailty
in the elderly makes it difficult to establish a protocol that
identifies the syndrome as a risk factor for osteoporotic fracture [10,11].
The phenotypic definition of frailty and the frailty index have been
shown to be independent risk factors for this type of fractures,
independent of chronological age. No literature has been found that
clarifies which of the two approaches to frailty syndrome allows greater
risk discrimination, since the existing studies are contradictory in
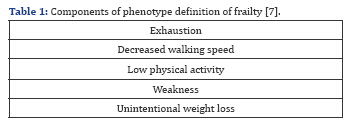
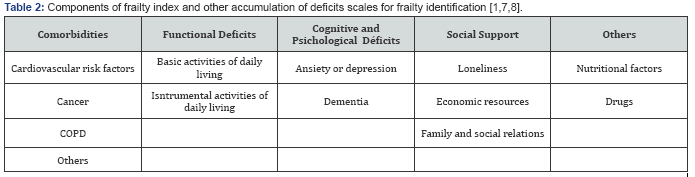
this matter [12,13]. Tables 1 & 2 shows the principal characteristics of these frailty models.
One of the tools most used in the calculation of
osteoporotic fracture risk is the fracture risk assessment tool (FRAX).
There is evidence that frailty index has the same predictive value for
osteoporotic fracture and hip fracture as this tool. Therefore, it can
be used as an aid to identify the risk of this type of fracture in the
elderly [14].
There is little scientific evidence about the
evolution of the frailty syndrome before and after an osteoporotic
fracture, as follow-up studies should be performed. It has been
demonstrated that frailty index and other accumulation definitions of
frailty shows greater frailty after a fracture, but this may be not
applicable as functional deficit is a logical consequence of a fracture [15].
Further research must be made in order to identify the evolution of
frailty in relation to a fracture, as frailty can be used as an
indicator for the effect of a treatment or intervention [8].
Conclusion
Detection of frailty in elderly women has been shown
to be useful for the assessment of the risk of osteoporotic fracture.
Due to the high prevalence of osteoporosis, as well as of frailty
syndrome, it is necessary to develop research on the influence of one in
the other over time, being frailty a good indicator of the effectiveness of treatments and interventions for osteoporosis [7].
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment