Juniper Publishers : Maternal Health-Seeking Behaviours in Preventing Preterm Delivery: A Case Control Study in Selangor
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Rosnah Sutan*
Abstract
Preterm delivery is a leading cause of new born
death especially in the developing country. It is one of the perinatal
outcome predictors of growth and survival of baby. The objective of this
study is to identify the relationship between mother's health seeking
behaviour during stages of pregnancy and preterm delivery. An unmatched
case control study was conducted at 34 selected primary care centres
(PHC) in Selangor from Mac to September 2013. Selection for case and
control groups from PHC was done using multistage random sampling based
on criteria set. All respondents were interviewed face-to-face by an
interviewer. A validated structured interviewed questionnaire was used
covering socio demographic, obstetric history, diet intake, stress
handling and physical activity. A total of 424 samples were obtained.
There were 212 of the postnatal mothers with preterm babies (cases) and
311 postnatal mothers with term babies (controls). This study found that
the Indian mother (aOR=2.54, 95% CI 1.30-4.98), young aged less than 20
years (aOR=4.89, 95% CI 1.07-22.29), primigravida (aOR=1.84, 95% CI
1.212.78), unplanned pregnancy (aOR=1.74, 95% CI 1.14-2.66) and not
taken folic acid during pre-pregnancy (aOR=2.21, 95% CI 1.01-4.84) was
found have higher risk for preterm delivery. Promoting reproductive
women to practice good health seeking behaviour by having regular folic
acid intake pre pregnancy and family planning, need to be strengthening
for further reduction of poor perinatal outcomes. Mothers need to
educate on self-monitoring and regular follow up to ensure safe
motherhood.
Keywords: Preterm delivery; Maternal health seeking behaviour; Pre pregnancy careIntroduction
Preterm birth is defined as the birth of a baby of less than 37 weeks gestation [1].
It is a major contributor (75%) to perinatal mortality and morbidity in
the world, as well as the primary risk factor for neurological damage
and disability [2].
The number of perinatal deaths is high and scientifically evidence
showed that it was due to preterm birth complications caused by
infection, asphyxia, hypothermia and hyper bilirubinemia [1].
Globally, an estimated 13 million babies are born premature every year,
with a premature birth rate of 5-7% in developed countries and a
premature birth rate of 9% in Asia [2].
The majority of premature incidences (85%) occurred in Africa and Asia
and this contributed to almost 11 million premature births [3].
Maternal health behaviours vary with the different
stages of pregnancy stages. It has an impact on pregnancy outcomes as
direct and indirectly. Research has proven poor maternal health
behaviours can cause low birth weight, premature birth, Sudden Infant
Death Syndrome (SIDS), and an increased risk of spontaneous abortion [4].
Most researches were carried out using existing clinical data from
patients' records in assessing the relationship between maternal health
behaviours and pregnancy outcomes. Many factors related to maternal
behaviour is unable to explore in depth using record data.
The main key challenges recorded in the Millennium
Development Goals 2015 of Malaysia 15 years achievement review has
recommended that the quality of care received by women before, during
and after pregnancy is the important elements for better child health
.this report has stated that the vast majority of child deaths in
Malaysia occur in the first year of life. A series of annual report from
Family Health Development Division of Malaysia has stated that between
1990 and 2007, neonatal mortality rates were halved to 3.8 per 1,000
live births but it increased slightly to 4.0 as of 2012. The leading
causes of under-five deaths in Malaysia by the ICD-10 classification are
conditions from perinatal period and mostly were due toimmaturity or
prematurity (36.5 per cent) [5].
Between 2008 and 2012, about 60- 65 per cent of deaths due to
prematurity had birth weights of less than 1000 grams. Between 54.5-63.7
per cent of these deaths occurred amongst the extreme preterm when the
period of gestation was less than 28 weeks. In order to improve maternal
health including perinatal health concerted effort to cover all
reproductive health women screening is highlighted and it should be
screen during pre-marital, pre-pregnancy care and all stages of
pregnancy care This care needs to incorporate aspects such as
reproductive health, family planning spacing and contraceptive use,
healthy diet and physical activity, optimal psychological and
psychosocial health [5].
The 11th Malaysia Plan and the
transformative 2030 global development agenda have been planned to cover
the Sustainable Development Goals to ensure that policies and
programmes are sustainable, resilient and inclusive to build a
foundation for improved quality of life for all in the country [5].
The important of awareness on health seeking behaviour for own health
has been emphasised in that plan. The aim of present study is to
identify the relationship between maternal health seeking behaviour at
pre pregnancy and during pregnancy stage with preterm delivery including
family planning practice, mother's intention on pregnancy, folic acid
intake pre pregnancy, stress handling, and physical activity using face
to face guided interviewed.
Materials and Methods
The methodology of present study has been described in an article published recently [6]
using same dataset but with different sub-analysis according to outcome
variable studied. In summary, this study was conducted in Selangor
which is located at the centre of west coast of Peninsular Malaysia.
Based on 2010 census, the state had a total population of 5.46 million
and was the second highest population growth in Malaysia [7].
The average population density in 2010 was 674 people per square
kilometre. The study was conducted in 34 randomly selected Primary
Healthcare Centres (PHC) out of 75 PHC in five selected districts with
highest populations in Selangor. An unmatched case-control study was
conducted. The study subjects were identified from the list of postnatal
mothers who had antenatal check-up in the selected PHC in Selangor. The
postnatal mothers with preterm babies (cases) and postnatal mothers
with normal term babies (controls) were recruited after met the
inclusion criteria: Malaysian, singleton, mothers with not known chronic
medical diseases or previous bad obstetric history, received antenatal
check-up at selected clinic and was recruited within 1 month
post-delivery. Pre term was defined as babies born alive at delivery
with estimated gestational age less than 37 weeks. Babies with no
gestational age recorded were not recruited for case group. Cases were
postnatal mothers who had preterm babies which were identified from
maternal home-based record registry at the clinics. Controls were
selected by systematic sampling using the list of postnatal mothers who
attended the same PHC as the case with gestational age at delivery ≥37
weeks recorded in the home-based record. The sample size was determined
based on previous study [8],
which was related to maternal occupation among preterm delivery. It was
calculated by Power and Sample Size 2 (PS2) based on Fleiss JL formulae
[9]. The calculation used the value of alpha=0.05, power of 80%, probability of exposure in the control (P0=71.9),
probability of exposure in case (P.^52.7) and the ratio of controls to
cases as 1:1. Fifteen percent was added for the expected non-response,
making the final sample size was 424 respondents. From the seven
districts in the Selangor, five districts were purposively selected as
they have the highest populations. The respondents were selected from 34
out of 75 PHC that shown highest antenatal attendance. The study was
conducted from March to September 2013. A validated structured
questionnaire was developed and administered to the participants through
an interview. The consistency of the content was controlled by using
only one interviewer. The questionnaire was developed by combining
different set of questionnaires from various sources with permission. At
present there in not known any specific questionnaire that can be used
to assess maternal health seeking behaviour along the pregnancy stages.
The questionnaire on nutritional domain and handling stress was adapted
from Health Promoting Lifestyle II [10] while the physical activity assessment was adapted from the Pregnancy Physical Activity Questionnaire (PPAQ) [11].
The questionnaire was first developed in English, and then translated
into Malay language. The questionnaire was pre-tested on ten postnatal
mothers in Universiti Kebangsaan Malaysia Medical Centre (UKMMC) who
were not included in the study.
The aim is to assess the face validity. A pilot study
was done among 100 postnatal mothers to examine the reliability and
construct validity of the questionnaire. The questionnaire contained two
sections. The first section covers the sociodemographic
characteristics, clinical data and delivery process as well as child's
health description. Data for the first section was obtained from the
maternal home-based record while the second section covers the maternal
health seeking behaviour across the pregnancy stages were collected
through an interview. The reliability (internal consistency) source of
information was tested using Cronbach's alpha reliability coefficients.
Cronbach's alpha coefficient was more than 0.7, an adequate level of
internal consistency of instruments. Data were entered using SPSS
version 21.0 for statistical analysis. Data exploration was done to
visualize the general feature of the data. After exploration, frequency
and percentages were used to assess the sociodemographic
characteristics, obstetric profile and pre-pregnancy and antenatal
behaviour. A logistic regression model was used to determine the
association between different factors and preterm delivery. All
variables were entered into bivariate analysis. In the multivariate
analysis, variables which p value was more than 0.2 were fitted into
multiple logistic regressions to predict factors of preterm delivery.
The strength of association was interpreted using the adjusted odds
ratio and 95% confidence interval (CI).
Ethical clearance was obtained from Medical Research
Etiquette Committee, Faculty of Medicine, UKMMC and National Medical
Research Register. Written consent through e-mail from the original
authors of the questionnaires used was obtained and modification was
done to accommodate with local people. Written consent was obtained from
the participants before the research. Moreover, the participants were
assured on the voluntarily and confidentiality of the information given.
Results
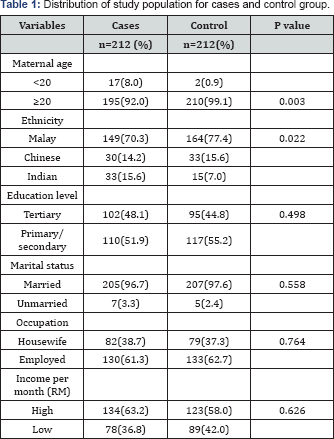
The total number of respondents participated were 424
postnatal mothers with 212 cases and 212 controls. The demographic
characteristic of respondents was summarized in Table 1 Both groups the
cases and controls were found not significant for education, marital
status, occupation and income per month. However, a significant
difference was noted for maternal age and ethnicity. Younger maternal
age group (8.0% cases and 0.9% controls) and the Indian (15.6 % cases
and 7.0% controls) were commonest among the preterm group.
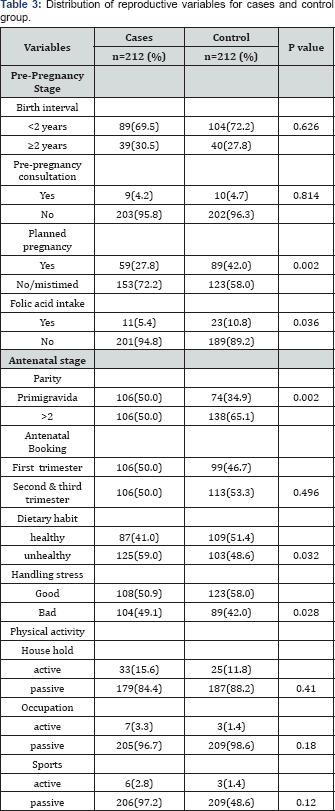
Pre pregnancy stage
Majority of respondents from both groups had birth
spacing of less than 2 years (69.5% cases and 72.2% controls). The
result depicted that the majority of respondents have unplanned or
mistimed pregnancies (72.2% cases and 58.0% of controls). Mistimed
pregnancy is defines as wanted pregnancy but get pregnant not at
suitable time. Majority of the respondents do not seek pre-pregnancy
consultation, either from the government nor private sector and only low
percentage (4-5%) for both groups received pre-pregnancy care
counselling. Taken folic acid supplement during pre-pregnancy is not
commonly practice. The finding showed a high percentage of not taken
folic acid supplement in both groups (94.8% cases and 89.2% controls).
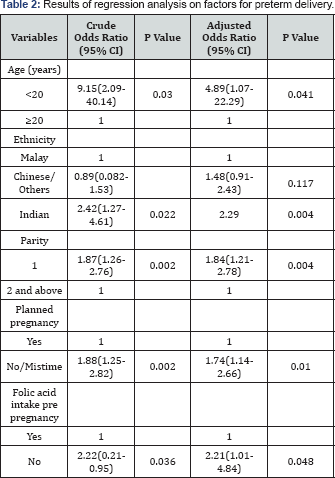
Bivariate analysis revealed that family planning and taking folic acid
supplement at prep regency stage has a direct and meaningful link to
preterm birth. Mothers who have unplanned or mistimed pregnancies have a
crude odds ratio of 1.88 (95% CI: 1.25-2.82) to experience a preterm
birth, compared to mothers who planned their pregnancies. Mothers who
practiced taking folic acid supplementation at pre-pregnancy have a
crude odds ratio of 2.22 (95% CI: 0.21-0.95) for preterm births compared
to mothers of controls group (Table 2).
Antenatal stage
During pregnancy, there are 3 variables that have a
meaningful link to preterm delivery: primigravida, poor nutrition, and
handling unhealthy stress (Table 3).
A mother who is primigravida has a crude odds ratio of as much as 1.87
(95% SK 1.26-2.76) more likely to experience a preterm delivery as
compared to a mother who is not primigravida (p value 0.002). Mothers
who practice poor nutritional habits have a crude odds ratio of as much
as 1.52(95% SK 1.04-2.22) with the p value=0.032. Mothers who passively
deal with stress have a crude odds ratio of as much as 1.43 (95% SK
1.03-1.97) (Table 2).
Predicted factors for preterm delivery
Multivariate logistic regression was conducted to
predict the final determinant of preterm delivery All variables with
p<0.25 in simple logistic regression were analysed. The following
factors are predictive of preterm delivery: mothers of Indian ethnicity,
primipara, unplanned pregnancy, not taking folic acid during
pre-pregnancy and younger mother. Table 3 shows the multivariate
analysis and it reveals that the group of mothers who are pregnant for
the first time, are 1.84 times more likely to experience preterm
delivery, as compared to mothers who are pregnant the second time or
more (adjusted odds ratio=1.84, 95% SK1.21-2.78). Mothers of Indian
ethnicity are more likely to experience preterm delivery 2.54 times when
compared to mothers of other ethnicities (adjusted odds ratio=2.54, 95%
SK 1.30-4.98). The third factor is family planning, where analysis
shows that mothers who do not plan their pregnancies are 1.74 times more
likely to experience preterm delivery as compared to those who plan
their pregnancies (adjusted odds ratio=1.74, 95% SK 1.14-2.66). The
fourth predictor of preterm delivery is the age factor. Mothers age
<20 years are 4.89 times more likely to have preterm delivery as
compared to mothers aged 20 and above (adjusted odds ratio=4.89, 95% SK
1.07-22.29). The fifth predictor is not taking folic acid during
pre-pregnancy stage whereby the result shows that mothers who do not
taken folic acid at pre pregnancy stage are at 2.21 times risk of more
likely to experience preterm delivery when compared otherwise (adjusted
odds ratio=2.21, 95% SK1.01-4.84).
Discussion
Mother's health seeking behaviour during
pre-pregnancy and antenatal stages has an influence on perinatal
outcome. Majority of research reveals that poor maternal health seeking
behaviour results in poor perinatal outcomes, such as premature birth
and low birth weight. This research differs from other researches
because the researcher interviewed every respondent, as compared to
other researches that use available data from hospitals. The main
objective of this research is to identify the link between the behaviour
in receiving maternal health care and preterm delivery. Results of the
research reveals five predictive factors contributing to preterm
delivery in Selangor that is: mothers of Indian ethnicity, mothers below
20 years of age, primigravida, not planned for the pregnancy and not
taken folic acid pre-pregnancy stage. The result of this research is
parallel to the research carried out at Hospital Seremban, which also
discovered that mothers of Indian ethnicity are most at risk when
compared to mothers of Chinese or Malay ethnicity [12].
Mothers below 20 years of age are 4.89 times more at
risk compared to a mother age ≥20 years. The outcome of this research is
supported by the meta-analysis of research done by Gibbs et al. [13] that states, a young mother has a risk of 1.68 times [13].
There are many theories that are often said to be linked to the risk of
young mothers and the perinatal outcomes, such as preterm delivery. A
popular theory is the competition for nutrients between mother and the
foetus in pregnancy [14].Other
theories explain that young mothers (aged 19 and below) have just
experienced puberty, therefore there is a biological impact on a
mother's growth, in which the mother's pelvic bone and height are
insufficient and interferes with the growth of the foetus she is
carrying. This causes the baby to be born earlier that date as compared
to a mother who is an adult [13].
There are also views that say mothers aged 19 and below normally lack
sufficient knowledge in preparing for pregnancy and the maternal
behaviour regarding health care pre-pregnancy and during pregnancy [15].
This research outcome is similar to earlier research
outcomes that say primigravida have a higher risk compared to mothers
with a multi para status [15-17].
Meta-analysis outcomes are used to research simultaneously the parity
effect and mother's age and find that these two factors are linked to
preterm delivery, that is mothers who are 18 years of age and
nulliparous, prove to be the group that has the highest risk compared to
other ages and parities. Therefore, present research finding is
parallel to the outcome of the meta-analysis outcome research that finds
both factors which are below 20 years of age and primigravida have a
high risk of premature birth [18].
Family planning status is one of the important
predictive factors to determine the likelihood of a preterm delivery,
that is, mothers who are not plan to be pregnant have higher risk of
1.74 times as compared to a mother who planned to be pregnant. The
outcome of this research is parallel to earlier researches which use
population data from PRAMS (Pregnancy Risk Assessment Monitoring
Surveillance) in the United States of America which also found that
mothers who do not intend or do not plan to be pregnant have a risk of
as much as 1.16 times as compared otherwise [19].
The outcome of the multivariate analysis reveals that
the practice of taking folic acid pre pregnancy has a meaningful link
to preterm delivery. Mothers who do not practice this have a risk of as
much as 2.21 of having preterm delivery as compared otherwise. There are
various researches that have different outcomes in relation to the
practice of taking folic acid during pre-pregnancy, that is, there are
researches carried out in Holland revealing that this practice only has a
meaningful link to low birth weight and not to preterm delivery [20]. The Sweden cohort research also found that there is no protective effect of folic acid against preterm delivery [21].
However, the dosage and duration of folic acid taken by the mothers
before pregnant, geographical conditions (home), as well as the mother's
own daily nutrition may need to be explore further as a micro increment
or decrease on a human body may play different role. Generally up to
this point, there still is no research that proves the practice of
taking folic acid during pre-pregnancy has any positive link in
preventing premature birth, but it has a weak correlation to the
increase in a baby's average birth weight, which is in tandem with the
latest meta-analysis of research [2223]. However, present study has proven it beneficial in Selangor Malaysia mothers who plan for future pregnancy
Conclusion and Recommendation
The present research reveals that 5 predictive
maternal health seeking behaviour such as family planning practice,
taking folic acid during pre-pregnancy, younger maternal age; Indian
ethnicity and primiparity are higher risk of preterm delivery. This
reveals that mother's health seeking behaviour during pre-pregnancy is
very important as it also has an effect in preventing preterm delivery.
Therefore, knowledge related to maternal behaviour in getting the right
health care during prepregnancy, especially in family planning, needs to
be emphasised among all groups of reproductive women especially the
first time pregnancy, younger age and Indian minority group through
health promotion that needs to be carried out in the community based and
further emphasizing at clinic based. As been recommended by WHO [24]
which stated that the important of bottlenecks faced identification by
countries in implementation of effective new born health interventions
at scale and their possible solutions. Therefore based on present study
findings, Malaysia must emphasize on pre-pregnancy care services
targeted to all reproductive age couple for screening and gain knowledge
in preventing bad maternal and perinatal outcomes.
This research has limitations, in which, it was only
carried out in Selangor, which was purposive. Therefore, it can only be
generalised to the population in Selangor. The data that was collected,
may also be subject to recall bias as the interviews were conducted
retrospectively, and there is a possibility past information may not be
remembered fully. In the future, this research may be carried out with
matched control group for age and ethnicity.
Acknowledgement
We acknowledge our respondents participation,
healthcare workers who helped during data collection process. We thank
to the UKM who granted for this study
Declaration
Author(s) declare that there is no conflict of interest. All authors are responsible for the content and writing of the paper.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Comments
Post a Comment