Juniper Publishers: Pregnancy Induced Hypertension and Associated Factors among Pregnant Women
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S
HEALTH
Journal of Gynecology and Women’s Health-Juniper
Publishers
Authored by Nazma Sultana*
Abstract
Pregnancy induced hypertension is a burning issue in
terms of maternal mortality and morbidity not only in Bangladesh but
also worldwide. Actually it is risk factor for both mother and child.
This cross sectional hospital based study was conducted to assess
prevalence of pregnancy induced hypertension and its determinants among
pregnant women attending teaching hospital in third trimester Non
probability purposive sampling was used to collect sample. Structured
questionnaire was used to collect data. Face to face interview was taken
as well as medical record was checked. Average age of the respondent's
26.03±5.77 years. More than half of the respondents completed SSC level
education. Average income of the respondent's was 33100.00±76135.29 BDT.
Three-fourth of the respondents had family history of hypertension.
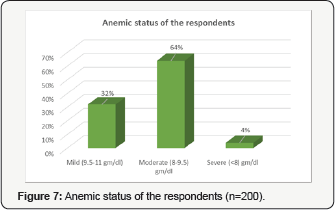
More than half of the respondents (64%) suffered from moderate anemia.
Average ANC visit was 4.43±1.58. Multipara, primipara and nullipara were
63%, 33% and 4% respectively. Underweight, normal, overweight and obese
were 4%, 28.50%, 26.50% and 41%. The prevalence of pregnancy induced
hypertension was 7.5%. Statistical significant association was found
between pregnancy induced hypertension and socioeconomic status. Further
large scale depth study can be conducted to get more precise result.
Keywords: Pregnancy induced hypertension; Associated factorsIntroduction
Pregnancy is a physiological phenomenon for most
women. However, some develop problems during its evolution, putting both
the mothers and the conceptus health at sake [1].
Gestational hypertension is the most common cause of hypertension in
pregnant women. Gestational hypertension is a clinical diagnosis defined
by the new onset of hypertension (systolic blood pressure ≥140mmHg
and/or diastolic blood pressure ≥90mmHg) at ≥20 weeks of gestation in
the absence of proteinuria or new signs of end-organ dysfunction [2].
The blood pressure readings should be documented on at least two
occasions at least four hours apart. Gestational hypertension is severe
when systolic blood pressure is ≥160 mmHg and/or diastolic blood
pressure is ≥110 mmHg on two consecutive blood pressure measurements at
least four hours apart [3-5].
Gestational hypertension is one of the maternal diseases that causes
the most detrimental effects to the maternal, fetal, and neonatal
organisms. This disease is responsible for high maternal and perinatal
morbidity and mortality rates, and is one of the main public health
problems [6,7].
According to the Health Ministry, hypertension during pregnancy,
depending on the severity level, is considered a risk factor, which,
associated with individual characteristics, unfavorable socioeconomic
conditions, certain obstetric histories and clinical problems could
trigger harms to the maternal-fetal binomial [8].
The hypertensive syndromes of pregnancy are the leading cause of
maternal and fetal morbidity and mortality in the developed world [9,10],
occurring in around 8% of pregnancies. Hypertensive syndromes are also a
cause of perinatal morbidity and mortality, mainly from intrauterine
growth restriction due to utero-placental insufficiency and
complications related to prematurity [11]. Even mild hypertension is associated with greater risk for prematurity and newborns who are small for gestational age [12].
Despite the severity of disease of both preeclampsia and gestational
hypertension, differences in risk factors between severe preeclampsia
and gestational hypertension may increase controversies over expectant
versus aggressive treatment, and there is insufficient literature on
Asian women with preeclampsia and gestational hypertension regarding the
issue of maternal complications [13].
Recent studies have indicated higher risk of PIH among women with
family history of hypertension, previous history of pregnancy induced
hypertension, pre-exciting diabetes, gestational diabetes mellitus,
maternal age ≥40 years, multiple pregnancies, nulliparity, and
pre-pregnancy obesity [14].
Some prior studies have suggested that higher pre-pregnancy body mass
index is associated with increased risk of gestational hypertension and
pre-eclampsia [15].
Gestational hypertension is still a little-understood entity.
Hypertensive disorders in pregnancy are common and their incidence
appears to be increasing. Gestational hypertension is an abnormality
causing striking maternal, fetal and neonatal mortality and morbidity
both in developed and developing countries. Gestational hypertension is
found in 5-10% of pregnancies in the world. Increase in caesarean
section, abruption of premature placenta, preterm delivery, low birth
weight, stillbirth, acute renal failure, and intravascular coagulation
were more frequently observed in women who developed hypertensive
disorders of pregnancy. The crude prevalence of systolic and diastolic
hypertension in pregnancy in rural area of Bangladesh was 6.8% and 5.4%,
respectively. It is proved that gestational hypertension and low birth
weight is well linked. So prevalence of gestational hypertension among
pregnant women in Bangladesh context specially urban based study in a
teaching hospital is an urgent need.
Materials and Methods
This cross sectional study was conducted at
conveniently selected at Ad-din Medical College & Hospital,
Keraniganj, Dhaka. This area was purposively selected to get adequate
sample. Study was run for three months from 1st September, 2016 to 30th
November, 2016. Non probability convenient sampling method was used on
the basis of inclusion and exclusion criteria. The study was mainly
based on primary data. It consists of both data gathered by structured
and semi structured questionnaires and in depth interviews with
Bangladeshi women. The socioeconomic scenarios of the respondents were
obtained. Blood pressure was measured by investigator herself. Medical
records were also verified. The respondents were selected consecutively
who meet the inclusion and exclusion criteria. Data were collected by
interviewer administered questionnaires. Questionnaires was comprised of
several topics, including sociodemographic background (age, educational
status, occupation, monthly income, etc.), blood pressure status and
BMI. After data collection, data were sorted and scrutinized by me and
then data were analyzed by SPSS version 20.0 program. The open ended
questions were grouped and categorized. Data were analyzed by
descriptive statistics and inferential statistics.
Results
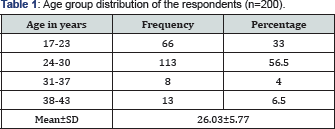
Table shows that mean age of the respondent's
26.03±5.77 years. More than half of the respondents represented 24-30
years age group followed by 17-23 years 33%, 31-37 years 4% and 38-43
years 6.5%.
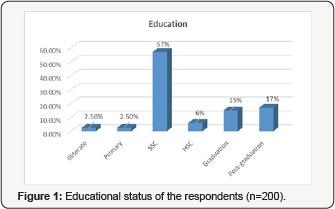
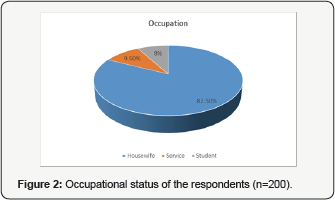
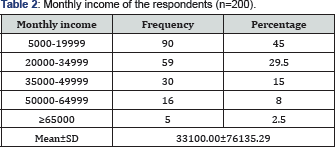
Table shows that average income of the respondent,s
was 33100.00±76135.29 BDT About 45%, 29.5%, 15%, 8% and 2.5% respondents
had monthly income 5000-19999 BDT, 20000-34999 BDT, 35000-49999 BDT,
50000-64999 BDT and ≥65000 BDT
Table 1
shows that mean age of the respondent’s 26.03±5.77 years. More than
half of the respondents represented 24-30 years age group followed by
17-23 years 33%, 31-37 years 4% and 38-43 years 6.5%. More than half of
the respondents completed SSC level education followed by
post-graduation 17%, graduation 15%, HSC 6%, primary 2.50% and
illiterate 2.50% (Figure 1). Housewife, service and student were 82.50%, 9.50% and 8% respectively (Figure 2). Table 2
shows that average income of the respondent's was 33100.00±76135.29
BDT. About 45%, 29.5%, 15%, 8% and 2.5% respondents had monthly income
500019999 BDT, 20000-34999 BDT, 35000-49999 BDT, 50000-64999 BDT and
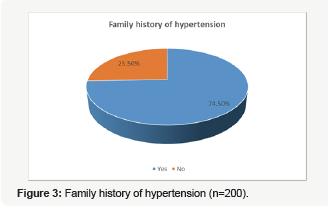
≥65000 BDT. Three-fourth of the respondents had family history of
hypertension whereas one-fourth had no family history of hypertension (Figure 3).
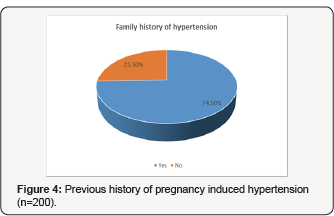
Almost 98% respondents had no previous history of pregnancy induced
hypertension whereas 2% had previous history of pregnancy induced
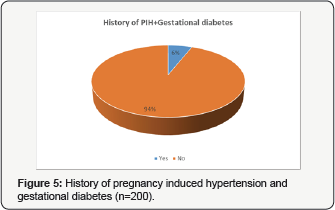
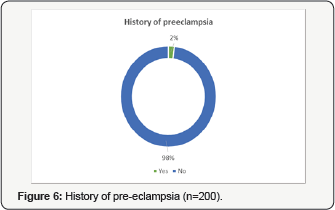
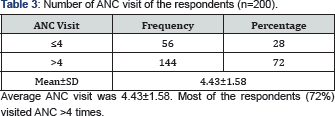
hypertension (Figure 4). Six percent pregnant women had history of both pregnancy induced hypertension and gestational diabetes (Figure 5). This doughnut shows 98% had no history of preeclampsia (Figure 6). More than half of the respondents (64%) suffered from moderate anemia followed by mild anemia 32% and severe anemia 4% (Figure 7). Table 3 shows Average ANC visit was 4.43±1.58. Most of the respondents (72%) visited ANC >4 times. Table 4
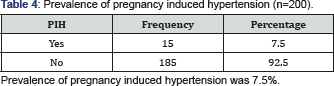
shows Prevalence of pregnancy induced hypertension was 7.5%.
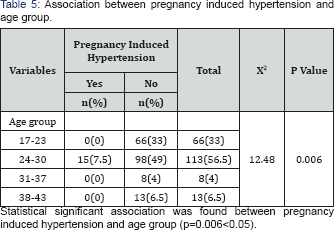
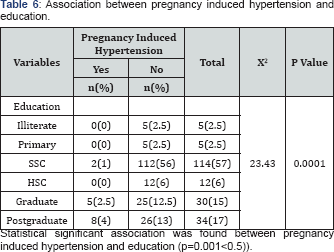
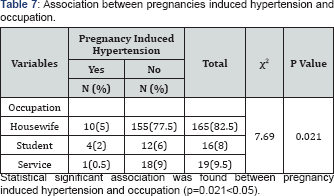
Statistical significant association was found between pregnancy induced
hypertension and age group (p=0.006<0.05) (Table 5). Table 6 shows Statistical significant association was found between pregnancy induced hypertension and education (p=0.001<0.5). Table 7 shows Statistical significant association was found between pregnancy induced hypertension and occupation (p=0.021<0.05).
Discussion
Pregnancy induced hypertension is thought to be one
of the major causes of maternal death and sufferings all over the
country. This study was conducted to know prevalence of pregnancy
induced hypertension in third trimester in a teaching hospital. The
prevalence of the hypertensive disorders in pregnancy was 7.5% in this
study but 21.6% and 17.2% that had been reported from south-eastern
Nigeria and Finland, respectively [16,17]. However, it was greater than 10% and 11.6% that had been reported from Ibadan and Benin City [18,19].
The factor that may be responsible for the low prevalence of
hypertensive disorder in our hospital could be due to time constraint
and small sample size. In this study, history of preeclampsia was 2%.
This disagrees with the 5-10% prevalence of other studies carried out in
Lagos, Ibadan, Calabar, Kano and other parts of the world [20-24]. The age and parity distribution of the cases in this study were also similar to those in other reports [25,26].
A positive family history of hypertension was found to be a significant
risk factor for developing HDP in this study. Women whose mothers
suffered from PIH were three times more likely to develop PIH than other
women [27,28].
Three-fourth of the respondents had family history of hypertension
whereas one-fourth had no family history of hypertension. Multiple
pregnancy, gestational diabetes and previous history of preeclampsia
were significant risk factors for developing HDP. This findings were
same as in other studies [29,30].
These are consistent with the hypothesis that immune maladaptation
might play a role in triggering the development of HDP. Almost 98%
respondents had no previous history of pregnancy induced hypertension
whereas 2% had previous history of pregnancy induced hypertension. Most
of the respondents (96%) did not have history of gestational diabetes.
It was also found that BMI >27kg/m2 was associated significantly with
the risk of the development of HDP. It has been observed that obese
women were more likely to have increased levels of serum triglycerides,
very low-density lipoproteins and formation of small, dense low-density
lipoprotein particles. Such lipid alterations have been suggested to
promote oxidative stress, caused by either ischaemia-reperfusion
mechanism or activated neutrophils and lead to endothelial cell
dysfunction [31].
More than half of the respondents (64%) suffered from moderate anemia
followed by mild anemia 32% and severe anemia 4%. Underweight, normal,
overweight and obese were 4%, 28.50%, 26.50% and 41%. Statistical
significant association was found between pregnancy induced hypertension
and socioeconomic status. A prospective study conducted by Bener and
Saleh revealed that obesity increased the odds of developing PIH by 10
times [32]. Obesity among women in Zimbabwe has increased from 1.2% in 2005 to 15.1% in 2010 [33,34]. Other studies have also shown that obesity is a risk factor for PIH [35,36]
hence if such women were to become pregnant, they would be at higher
risk of developing PIH. Compared to the recommendations by the World
Health Organization (WHO), the caesarean section delivery rate of 12.5%
is above the recommended cut off. WHO recommends caesarean section rates
between 5% and 10% and rates of 15% are considered to do more harm than
good. Literature suggests that cesarean section rates higher than the
proposed 15% upper threshold are associated with increased morbidity and
mortality for both mothers and babies [37].
A population-based retrospective cohort study conducted in Zhejiang
province in China in 1995-2000 demonstrates the importance of use of
cesarean section during delivery among women with PIH. It was found that
moderate and severe PIH early developed during pregnancy could increase
the risk of perinatal mortality while the cesarean delivery could
decrease the risks in women with PIH [38].
In our study, however, it was not noted that among the reasons for
caesarean section. Possible selection bias among women recruited into
this study cannot be ruled out. The study was conducted over a short
period of time thus we could have missed essential characteristics among
women who did not get the chance to be part of this study.
Conclusion
The prevalence of pregnancy induced hypertension was
7.5%. Average age of the respondent's 26.03±5.77 years. More than half
of the respondents completed SSC level education. Average income of the
respondent's was 33100.00±76135.29 BDT. Three-fourth of the respondents
had family history of hypertension. More than half of the respondents
(64%) suffered from moderate anemia. Average ANC visit was 4.43±1.58.
Statistical significant association was found between pregnancy induced
hypertension and age group, education and occupation.
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s
Health please click on: https://juniperpublishers.com/jgwh/




Great.
ReplyDeletehttps://forums.matterhackers.com/user/jackswann
Great post.
ReplyDeletehttps://logopond.com/StephenDowdy/profile/459214/?filter=&page=