Juniper Publishers: Biosensors, the Emerging Tools in the Identification and Detection of Cancer Markers
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S HEALTH
Journal of Gynecology and Women’s Health-Juniper Publishers
Authored by Muhammad Torequl Islam*
Abstract
The cancer is chaos, causing impairment by biochemical pathways in a biological system. Mulfunctioning of cells throughout the human body is mostly observed in cancer and is still the outmost lethal disease in the world. There is a difference in expression of parameters within a host during its normal physiology and pathological conditions, those are identified and detected to proceed on for the treatment. A number of conventional methods are available nowadays, despite of their potential limitations. Biosensors, the analytical devices that convert biological responses into electrical signals are now popularly used in many fields such as food industry, metabolic engineering, plant biology, marine science, defense, drug discovery and development. Beside these, in the medical sectors, their important roles are remarkable, especially in the early detection of a disease, and monitoring the therapeutic progression and disease state. To date, diagnostic tests by using biosensors for the early detection of cancer biomarkers are available; these provide noninvasive/minimally invasive assays with high through output and patient survival rate. This paper reviews an overview on biosensor-implementation in some cancers along with their future applicability.
Keywords: Biomarker; Biosensor; Cancer; Diagnosis
Abbreviations: 18F-FDG: 18F-Fluorodeoxyglucose; AFP: Alpha-Fetoprotein; AKT: Protein Kinase B; AMARC: Methylacyl Alpha CoA Racemase; AuNPs: Gold Nanoparticles; B2M: Beta-2-Microglobulin; BRAF: B-Raf; BRCA: Breast Cancer Associated Gene; CA: Cancer Antigen; CAPB: Cocamidopropyl Betaine; CD: Cytotoxic T Cell; CEA: Carcinoembryonic Antigen; CGH: Comparative Genomic Hybridization; CK: Creatine Kinase; CRP: C-Reactive Protein; CTC: Cutaneous T Cell; CYFRA: Cytokeratin Fragment; DD3: Discoidin Domain 3; DDR2: Discoidin Domain Receptor 2; DCIS: Ductal Carcinoma In Situ; DEPDC1: N,N-Diethyl-1,4-Phenylene Domain Containing 1; Dsdna: Double-Stranded DNA; EGFR: Epidermal Growth Factor Receptor; ELAC2: Elac Ribonuclease Z 2; ELF: Epithelial Lining Fluid; ELISA: Enzyme-Linked Immunosorbent Assay; EPCA: Early Prostate Carcinoma Antigen; Epcam: Epithelial Cell Adhesion Molecule; ER: Estrogen Receptor; EXO1: Exonuclease 1; FISH: Fluorescence In Situ Hybridization; FOXM1: Forkhead Box Protein M1; HAPLN1: Hyaluronan And Proteoglycan Link Protein 1; HE4: Human Epididymis Secretory Protein 4; HER2: Human Estrogen Receptor 2; HfO2: Hafnium Oxide; HPC: Haematopoietic Progenitor Cell; HPC1: Haematopoietic Progenitor Cell 1; HPCX: Haematopoietic Progenitor Cell X; HPV: Human Papillomavirus; IHC: Immunohistochemistry; IL: Interleukin; IUPAC: International Union of Pure and Applied Chemistry; KEAP1: Kelch-Like ECH-Associated Protein 1; KRAS: K-Ras; LDCT: Low-Dose Computed Tomography; M-CSF: Macrophage Colony-Stimulating Factor; Mirna: Micro Ribonucleic Acid; MRI: Magnetic Resonance Imaging; MUC1: Mucin 1; NCI: National Cancer Institute; NFE2L2: Nuclear Factor, Erythroid 2 Like 2; NUSAP1: Nucleolar And Spindle Associated Protein 1; P53: Protein 53; PCAP: Pulmonary Capillary Pressure; PET: Positron Emission Tomography; PIK3CA: Phosphoinositide 3-Kinase Catalytic Subunit Alpha; PNA: Peptide Nucleic Acid; PR2: Progesterone Receptor 2; PSA: Prostate-Specific Antigen; PTEN: Phosphatase and Tensin Homolog; QCM: Quartz Crystal Microbalance; QDs: Quantum Dots; Qpcr: Quantitative Polymerase Chain Reaction; RT-PCR: Real-Time Polymerase Chain Reaction; Real-Time qrt-PCR: Real-Time Quantitative Reverse Transcription PCR; RRM2: RNA Recognition Motif 2; SPP1: Secreted Phosphoprotein 1; SPR: Surface Plasmon Resonance; Ssdna: Single-Stranded DNA; TATI: Tumour-Associated Trypsin Inhibitor; TNF: Tumor Necrosis Factor; TPA: Tissue Plasminogen Activator; TPS: Thermoplastic System
Introduction
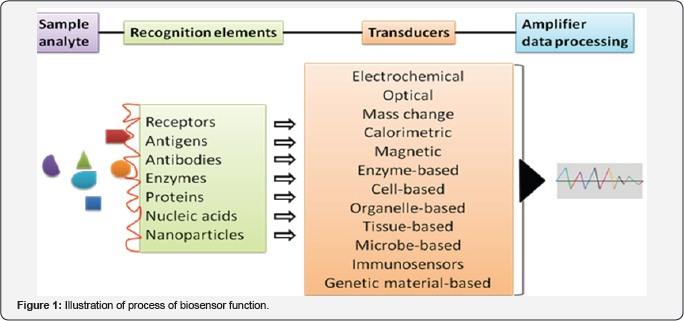
Evidences suggest that an increasing number of attentions have been focused on developing rapid techniques called 'biosensor technology' for the identification, detection and monitoring of human health-related conditions. The biosensors are the bioanalytical devices, incorporating molecular recognition together with physicochemical transducers, for the analysis of biomarkers. The term "biosensor” was first used by Cammann [1] and its definition was introduced by the International Union of Pure and Applied Chemistry (IUPAC) [2]; finally started the journey in the 1960s by the pioneers Clark and Lyons. A biosensor connects chemistry, biology, and engineering in its fabrication. Based on the mechanism, the materials used in biosensors are: biocatalytic group comprising enzymes, bio affinity group, including antibodies, antigens and nucleic acids, and microbe-based containing microorganisms. Till date, different types of biosensors are: enzyme-based; microbe-based or cell-based; tissue-based; immunosensors; protein, DNA or genetically-encoded biosensors; electrochemical, magnetic, optical, thermal and piezoelectric biosensors. Each biosensor has a conformation and uniqueness in its fabrication and application. A common illustration of the function of biosensor has been shown in Figure 1.
The applications of biosensors are growing day by day. Till date, they can be found in- food and fermentation industry, plant biology, in defense, marine science, drug discovery and medical sciences.
In the diagnostic centers, glucose biosensors are widely used for the detection of blood-glucose levels [3]. Biosensor, based on hafnium oxide (HfO2), is used for the detection of human interleukin (1L)-10 [4] in cardiovascular patients. Biosensors are also engaged in the diagnosis of infectious diseases and anti-microbial susceptibility. Other important applications of biosensors include: quantitative measurement of cardiac markers in undiluted serum, microfluidic impedance assay for controlling endothelin-induced cardiac hypertrophy, immunosensor array for clinical immunophenotyping of acute leukemias, effect of oxazaborolidines on immobilized fructosyltransferase in dental diseases; histone deacylase (HDAC) inhibitor assay from resonance energy transfer, biochip for a quick and accurate detection of multiple cancer markers and neurochemical detection by diamond microneedle electrodes.
According to the National Cancer Institute (NCI), United States 2015 report approximately 1,658,370 new cases of cancer have been diagnosed and 589,430 deaths. The literature says that, in human the most common cancers are: breast, lung, bronchus, prostate, colon, rectum, skin melanoma, Hodgkin lymphoma, thyroid, liver, renal pelvis, endometrial, leukemia and pancreatic cancer [5]. It is doubtless that, the cancer is a multifactorial molecular disease that includes multistage development of tumor cells, caused by a range of genetic or environmental factors, such as exposure to carcinogenic chemicals or radiation, or has a microbiological cause, including bacterial (e.g. - stomach cancer) or viral (e.g. - cervical cancer) infection. In this context, promoter proliferative signaling, escapes from growth suppressors, resistive cell death, replicative immortality, triggering of angiogenesis, and activation of invasion and metastasis are occurring along with the genomic instability, inflammation, and epigenetic changes. Thus, determination of responsible genes, proteins, and abnormalities in the tumor and body fluids such as blood, urine and sputum in the early stage is crucial for an effective treatment.
Microarrays, quantitative polymerase chain reaction (qPCR) and enzyme-linked immunosorbent assay (ELISA) are the frequently used detection methods in cancers. The common disadvantages of these techniques are: expensive, requires highly qualified personnel, time consuming, laboratory-dependent, difficulty in handling, tissue oxidation (qPCR), limited access, destructive testing (microarrays), lack of flexibility in selecting standards, quality and sampling amount [6]. Although, biosensors have limited use in clinics and the molecular markers are not reproducible, but they can overcome other limitations as said above. Moreover, the in situ application, high analytical specificity, cost-effectiveness in time and material consumption, sensitivity through automation, integration of multiple processes in a single device, low-space occupancy and multi-analyte testing capability are the major causes of increasing popularity of biosensors [7,8].
This text focuses a brief scenario on biosensors involvement and applicability in the monitor and detection of early cancer development. Additionally, the hopes and challenges are also plugged in.
Designing of biosensors for early cancer detection
To monoclonal antibodies and aptamers (oligonucleotide or peptide molecules that bind to a specific target molecule) are often used to capture cancer agents, including antigens, while micro ribonucleic acids (miRNAs) corresponds single stranded desoxyribonucleic acid (ssDNA). The transducer, in a biosensor converts the molecular recognition signal to an electrical signal. It may be electrochemical (potentiometry, amperometry, conductometry/impedimetry), optical (fluorescence, luminescence, colorimetric and interferometry), calorimetric (thermistor) or based on mass changes (piezoelectric/ acoustic waves) [9] (Figure 1).
The electrochemical biosensors detect an electrical response when there is a molecular recognition of a specific element. For an example- detection of cancer marker hPRL-3 in breast cancer cells [10]. By utilizing specific DNA sequences, it is possible to recognize elements in cancer and/or conjoined with genetic mutations. BRCA1 and BRCA2 mutations are associated with hereditary breast cancer. This type of biosensor has the ability to detect damaged DNA and carcinogens associated with the damage [11]. Moreover, by using multiple sensors with multiple transducers, it is also possible to detect multiple factors associated with a particular cancer. The cytosensors are the electrochemical-cell-based biosensors utilize living cells as a biological recognition element [12].
Optical biosensors measure the changes in specific wavelengths of light [13]. The biosensors with photonic crystals can capture the light areas or very small volumes and transmit the light to a high electromagnetic field to display the result. These types of biosensors are implemented for monitoring changes in proliferation and apoptosis of breast cancer cells, the rate of drug cytotoxicity and understanding the effectiveness of the treatment. Optical biosensor based on laser-induced fluorescence is evident to use in the diagnosis and monitoring of throat cancer. Interestingly, the use of this biosensor prevented surgical biopsies and the pain associated recovery in more than 200 patients [11].
The mass change biosensors e. g. -piezoelectric biosensors measure the changes in resonance frequency of a piezoelectric crystal in the manner of changing mass on the crystal structure. By using these biosensors coupled with polymerase chain reaction (PCR) amplifications, it is possible to detect the point of mutations in the human p53 gene.
The use of calorimetric biosensors is rarely in the diagnosis of cancer. They measure exothermic reactions. However, in a study with gold nanoparticles (AuNPs), calorimetric biosensors successfully detected two different types of cells in acute leukemia and cells in Burkitt's. Wang et al. [14] suggested that 2D nanomaterial-based biosensors can be used to detect cancer biomarkers. These, mainly cover the graphene, grapheme derivatives (i.e. -grapheme oxide and reduced grapheme oxide), and graphene-like nanomaterials (i.e. -2D layered transition metal dichalcogenides, graphite carbon nitride and boron nitride nanomaterials).
The enzyme-based biosensors have been devised on immobilization methods, i.e. adsorption of enzymes by chemical bonding such as Van der Waals forces, ionic or covalent bonding. The commonly used enzymes for this purpose are oxidoreductases, polyphenol oxidases, peroxidases, and amino- oxidases [15]. The analyte of the tissue-based biosensors are the inhibitors or substrates, including amino acids. On the other hand, the organelle-based biosensors are used to detect the membranes, chloroplasts, mitochondria, and microsomes. Immunosensors act through an interaction between antibodies with their specific antigens. In this case, the antibodies specifically bind to pathogens or toxins, or interact with components of the host's immune system. The microbe-based biosensors detect the microorganisms (both live and dead) or their liberated materials, while DNA biosensors are devised on the property that single-strand nucleic acid molecule is able to recognize and bind to its complementary strand in a sample. In the latter case, an interaction occurs by the formation of stable hydrogen bonds between the two nucleic acid strands [16]. The magnetic (miniaturized) biosensors detect magnetic micro- and nanoparticles in microfluidic channels using the magnetoresistance effect [17]. These can be also applied for the detection of microorganisms.
Biosensor-detectable biomarkers in some cancers
Malignant cells produce biological substances, including pro-inflammatory and inflammatory mediators. Moreover, a number of intra- and intercellular compounds, such as hormones, mucin, isoenzymes, oncogenes, oncofetal antigens, tissue-specific proteins, circulating ribonucleic acids, and some glycoproteins and glycolipids are also the indicators of cancer [18,19]. Some of these markers are organ specific, while others are common. For example, neuron-specific enolase and a breast cancer gene are specific for lung and breast car-cinomas, respectively; whereas cancer antigen 15-3, cancer antigen 125 and carcinoembryonic antigen may be found in breast, lung, or colon cancer. More complications are seen in the expression of miRNAs in some diseases. Otherwise, biomarkers can show different concentration level in different type of cancer [20]. The hysiology, gender and racial factors also have an influence on the levels of a certain or group of biomarkers. Techniques used for biomarkers identification and detection are shown in Box 1.

Gene biomarkers have more specificity in cancers due to the genome diversity. A number of genes have been linked to somatic mutations in human tumor cells or tissues, including oncogenes and tumor suppressor genes, as well as genes encoding proteins that perform key functions in regulation of the cell cycle, DNA repair, and enzyme activity. For example, protein 53 (p53) gene, which is located on the short arm of the chromosome 17 in the human genome and is thought as a guardian of the genome, as it regulates the cell cycle and functions as a tumor suppressor [21]. However, a single mutation in the same location can initiate different cancers depending on the geographical location, ethnic back-ground, and/or gender of the patient. For an example, p53 proline mutation has been found to link in pancreatic cancer in males [22], which has been found to decrease the risk of breast cancer in Arab women [23].
The location of the mutation is also related to the situations of a particular cancer, such as codon 273 mutation in non-small cell lung cancer, while codon 248 for small cell lung cancer in the p53 gene [24]. The other detectable target may be the epidermal growth factor receptor (EGFR), responsible for tumor invasion, angiogenesis, cell proliferation, and apoptosis [25].

Genomic and proteomic analyses are performed to determine potential biomarkers, since the combined data are much more reliable and precise than the data obtained using a single methodology and helpful to find out more specific gene or protein biomarkers for a particular cancer type [26,27]. In protein chip biomarkers, the proteins are isolated and printed on a single slide surface can investigate protein profiling and antibodies via protein-protein interactions [28]. On the other hand, post-genomic technologies and bioinformatics tools are helpful to detect gene expression, mutations, single nucleotide polymorphisms, and cancer biology [29]. Till date, a number of biosensors have been introduced to detect cancer (some of them are shown in Table 1. An electrochemical molecular beacon biosensor has been developed for the sequence-specific recognition of DNA for cancer diagnosis and gene therapy, while the molecular beacon-based biosensors can be used to detect protein biomarkers, small molecules, and RNA . Double stranded DNA biosensors are capable to quantify within the range of 350 pM to 25 nM [30]. Potentiometric biosensors combining the effect and specific molecular imprinting can be used to detect cancer, carcinoembryonic antigen, discriminate between damaged and normal fibrinogen in bleeding disorders, and conformational changes in the protein [31]. Hyaluronan and proteoglycan link protein 1 (HAPLN1) can be used by using an electrochemical open-circuit potential method [32]. On the other hand, piezoelectric biosensor was developed to detect the prostate-specific antigen (PSA) and alpha-fetoprotein (AFP). A titanate zirconate ceramic resonator could success-fully detect PSA and AFP up to 0.25 ng/mL in a short time (30 minutes) with a small sample volume (1 µL) [33].
Nanoparticles have a wide range of applications for detection of different types of disease, such as cancer, infec-tious diseases, and neurological disorders [34]. Short fragments of DNA can be tagged with AuNPs for the detection of targeted gene sequences. On the other hand, quantum dots (QDs) and magnetic iron oxide nanoparticles can be designed for dual-mode imaging of cancer. The silica and iron oxide nanoparticles can be used to detect lung cancer cells [35]. AuNPs-conjugated anti-EGFR antibodies are evident to show 600% higher binding affinity with cancerous cells than noncancerous cells [36]. Manganese oxide nanoparticles combined with magnetic resonance imaging (MRI) can be used to diagnose neurological disorders such as Parkinson's disease, stroke, and Alzheimer's disease [37]. Moreover, there is a chance to attach the affinity ligands such as antibodies to these nanoparticles. The later type of fabrication can detect bacteria, while silver nanorods have been introduced for a rapid quantification and characterization of viruses, by recognizing spectral differences between viral strains, viruses, and viruses with gene deletions in biological samples [38]. The multicolor optical coding using QDs is also another important application in molecular diagnosis [39]. On the other hand, bio conjugated QDs are useful to detect disease progression, and response to therapy [40].
The ovarian cancer exhibits a wide range morphologies and variations in clinical and genetic ways during the process of tumor progression. In this cancer, the beta-2-microglobulin (B2M) is found to over express, that can be a useful tool to detect [41]. However, targeting of a single molecular marker is not enough [42]. In breast cancer, the detection of hormone receptors, such as estrogen (ER), progesterone receptor 2 (PR2) and the EGFR is commonly done. Although, the immune histochemistry (IHC) is used as a quantitative method to detect the expression of HER2 receptors, but is has some disadvantages in fixing protocols, registration systems and level of placement, and the selection of antibodies [43]. On the other hand, in cervical cancer the expression of the E6, E7 and E5 of the high-risk subtypes of human papillomavirus (HPV) oncoproteins can be measured in cervical cancer Although, it requires long periods of latency for the malignant transformation [44], but can be detected using a novel leaky surface acoustic wave peptide nucleic acid biosensor with double two-port resonators.
The linear discriminatory analysis, microarrays and RealTime Quantitative Reverse Transcription PCR (Real-Time qRT-PCR) have been used for the diagnosis of prostate cancer with 100% accuracy [45]. The AMARC (methylacyl alpha CoA racemase), an enzyme involved in the oxidation of branched chain fatty acids, which is evident to overexpress in prostate and some other cancers. In this regard, IHC antigen P504S is helpful to detect AMACR. Additionally, the blood and urine samples are also useful to detect the gene mRNA of AMACR using qRT- PCR, while the nuclear matrix protein, early prostate carcinoma antigen (EPCA) by using ELISA or tissue IHC [46].
In lung cancer, low-dose computed tomography (LDCT) is widely used [47]. A combination of computed tomography and positron emission tomography with 18F-fluorodeoxyglucose (18F-FDG PET/CT) is also used in this case. Generally, the growth of a tumor is accompanied by changes in genes and proteins. Thus the point of methylation or mutations of DNA, RNA and protein expression can be targeted. Some other biomarkers can also be helpful in this purpose, such as altered carbohydrates, cytokines and chemokines, volatile organic compounds from the peroxidation in the cell membrane [48]. In lung cancer, the other mutations can be detected as: BRAF [49], KRAS [50-52], HER2 [53,54], DDR2, PIK3CA, PTEN, AKT, KEAP1, and NFE2L2 [55]. Furthermore, recurrent gene rearrangements involve: ALK, ROS1, RET and NTRK in this cancer [56,57].
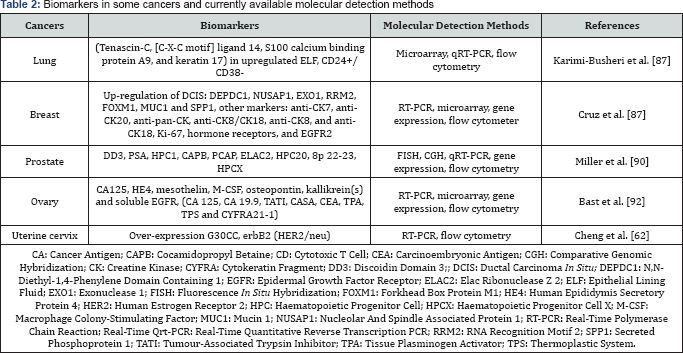
The AFP is a normal serum protein synthesized by liver, yolk sac and gastrointestinal tract. Over expression of AFP, is evident to cause liver cancer [58]. On the other hand, C-reactive protein (CRP), synthesized by IL-6 in the liver, circulates in the blood is a prognostic indicator of gastric cancer [59-65]. These types of biomarkers can be detected in serum by using electrochemical and quartz crystal microbalance (QCM) techniques. In breast cancer the detectable biomarkers are: ER, PR, HER2, BRCA1, Ki67, osteopontin, mammoglobin, sirtuins, autoantibodies,CA15-3, CA27.29, CTC, CEA, BRCA1, BRCA2, MUC1, EpCAM,EGFR, miR-21, 16, 27a, 150, 155, 191, 222. In Table 2, a list of biomarkers in some cancers has been shown along with the molecular detection methods [66-76].
Concluding remarks
With the biosensor and molecular techniques, it can be said that a number of molecular markers available may be excellent candidates for the identification and detection by using biosensors. Moreover, the use of biosensors in the early detection of cancer and monitoring the overall progress of disease state is the hopeful keys for the effective treatment, thus reducing the mortality rate of the patients [77-80]. Biosensors can be used in some laboratory tasks, including genotoxic and mutagenic markers such as chromosomal aberrations and micronucleus tests [81-85].
Doubtless, before treatment- proper diagnosis is essential. In this sense, still there is a long way to go to understand a complete set of markers in a particular cancer. Non-specificity in expression of some markers may offer wrong diagnosis, therefore, wrong treatment [86-90]. Otherwise, the problems in the reproducibility of the method and difficulties in the fabrication of the biosensor materials are also should be resolved. The level of detection is another fact in this novel technology, as the expression of biomarkers depends on: duration of disease, patient's pathophysiology, age, gender, genetic diversity, the conditions for taking of tissue, lifestyle of the patient, earlier and concurrent treatment received and so on.
However, continuity in research may be helpful to overcome the overall challenges those are yet to be resolved with the application of the biosensor in cancers. Finally, it is doubtless that, the biosensor technology has opened a hopeful door in the diagnosis, therefore earlier treatment- thus the possibility of an increase in the survival rate or lifespan, by decreasing suffering and mortality rate of the cancer patients [91-95].
For more open
access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s Health please click on: https://juniperpublishers.com/jgwh/
To read more......Fulltext in Gynecology and Women’s Health in Juniper Publishers
https://juniperpublishers.business.site/




Comments
Post a Comment