Juniper Publishers : Group B B-Hemolytic Streptococcus Screening and Treatment in Postpartum Endomyometritis
JUNIPER PUBLISHERS- JOURNAL OF GYNECOLOGY AND WOMEN’S HEALTH
Journal of Gynecology and Women’s Health-Juniper Publishers
Authored by Ara Dadivanyan*
Abstract
Introduction: The value of antenatal screening for Group B b-hemolyic streptococcus has been documented to significantly reduce the incidence of neonatal sepsis. The purpose of this study is to determine the impact of this antenatal screening on maternal outcome, specifically Group b streptococcus (GBBS) associated post partumendomyometritis.
Methods: Endometrial cultures were obtained from patients with endomyometritis prior to placement in one of three randomized antibiotic comparison protocols. Cultures were collected at time of diagnosis of endomyometritis, and then repeated following antibiotic regimen completion or alteration, and compared to matched, randomly selected patients.
Results: Of the 232 patients involved in the antibiotic studies, 31 (13.4%) had GBBS on initial endometrial culture, and were compared with 31 case- matched, randomly selected patients. Sixteen percent (16%) of those patients with GBBS associated endomyometritis had positive antenatal screening cultures and were subsequently treated. The prenatal course of those with GBBS associated endomyometritis was more frequently complicated by preterm delivery (25.8% vs9.6%). The range of isolated additional organisms was similar in both groups. Following antibiotic treatment of endomyometritis, 23 of 62 (37.1%) patients had enterococcus and 14 of 31 (45%) patients had GBBS on post-therapy endometrial cultures. Those patients with GBBS associated endomyomeritis had a greater number of major post-operative complications, especially if there was persistence of GBBS, versus patients in the control group.
Conclusion: Antenatal screening and treatment does not eliminate GBBS maternal complications. Those patients with GBBS endomyometritis deserve careful observation for serious post-operative complications.
Abbrevations: GBBS: Group B Hemolytic Streptococcus V
Introduction
Group B hemolytic streptococcus (S. agalactiae) is familiar to obstetricians/gynecologists and neonatologists as an important cause of neonatal infection. It frequently colonizes the female genital tract via contamination from its primary reservoir, the gastrointestinal tract. Many pregnant patients colonized with this organism deliver infants who are also colonized. Infection of the neonate with Group B b-hemolytic streptococcus (GBBS) can result in sepsis and shock, pneumonia, meningitis with permanent neurological sequelae, and occasionally death [1-4]. Maternal colonization with GBBS has been associated, but not conclusively proven to cause several maternal complications, including preterm labor,rupture of membranes, endometritis, pyelonephritis, and bacteremia [5-9]. It is one of the most frequently isolated organisms in bacteremic patients and is a known pathogen in puerperal septicemia.
Early antenatal screening for GBBS colonization and treatment remains controversial due to the high rate of recolonization and spontaneous conversion to a non-carrier state in others [2,8,10]. However, screening performed late in pregnancy often fails to protect those most at risk for infection, the premature fetus.
In a study by Watts, [4], it was demonstrated that isolation of GBBS at delivery was significantly associated with the development of postpartum endomyometritis. Therefore, an assumption may be made that the elimination of GBBS during the peripartum period would eliminate the GBBS associated postpartum endomyometritis. Therefore, we prospectively screened for GBBS and treated in the peripartum period. Those patients who developed endometritis were then evaluated to ascertain the presence or absence of GBBS, and the associated complications.
Methods and Materials
All patients seen in the first or second trimester were screened for GBBS utilizing previously published methods [9]. Patients who were found to have GBBS were treated with a regimen of oral ampicillin 500 mg every 6 hours for 7 days or cephalexin 500mg every 6 hours for 7 days, if penicillin allergic. Partners were not treated. Patients were re-screened in the third trimester, and retreated if found to be positive. All patients admitted for preterm labor or PROM were also screened. Following delivery by cesarean section, all women with clinical evidence of postpartum endomyometritis as defined by previously published criteria [10] were randomized to one of three prospective randomized antibiotic trials for the treatment of endomyometritis. The antibiotic regimens included meropenem 500 mg intravenously every 8 hours, cefmetazole 2 grams every 8 hours vs cefoxin 2 grams intravenously every 6 hours and trospectomicin 500mg/ aztreonam lgram intravenously every 8 hours.
Those excluded from these studies included patients:
a. Less than 18 years of age,
b. Antibiotic allergy to imipenems, cephalosporins, clindamycin, penicillins, or aminoglycosides,
c. History of seizure disorders,
d. Active liver or kidney disease, and
e. Breast feeding. All gave written informed consent. The study was approved by the hospital Institutional
Review Board
Once the diagnosis of postpartum endomyometritis was established, endometrial cultures and urine cultures were obtained. Endometrial samples were obtained using an aspiration suction curette as previously described. Repeat endometrial cultures were obtained prior to discharge, or at time of change in the antibiotic regimen following declaration as a treatment regimen failure. The chart of those having GBBS on initial endometrial culture (31) was reviewed. A control group of 31 patients with endomyometritis without GBBS on initial endometrial culture was then case-matched from the remaining group of patients.
Parameters assessed included:
a. Gravity, parity and age,
b. Results of prenatal pelvic culture for Group B streptococcus; if positive, the antibiotic used for treatment and results of the follow-up culture,
c. Results of prenatal urine cultures; if positive the organism involved, antibiotic for treatment and results of follow-up culture,
d. WBC count on admission and at time of antibiotic start,
e. Complicating factors such as premature rupture of membranes (PROM) , preterm labor (PTL), sexually transmitted diseases, cultures from endometrial samples,
f. Organisms before and after antibiotic treatment,
g. Presence and absence of treatment success and major post-operative complications and
h. Antibiotics used in treatment.
Results
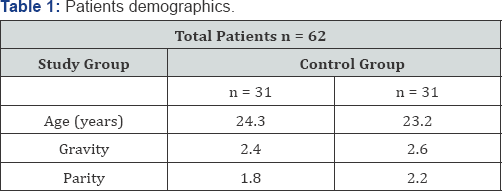
Of the 232 patients enrolled in the endometritis studies, 62 underwent chart review (31 with GBBS on endometrial culture and 31 case matched randomly selected controls). Demographic data for the groups are listed in Table 1. There was no statistical difference in the study patient populations.
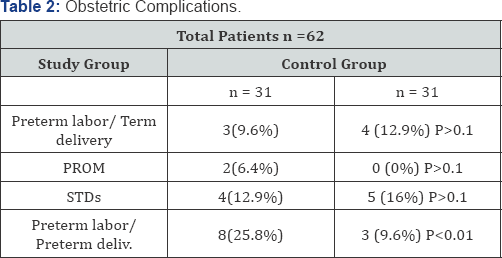
The prenatal course of patients in the GBBS endometritis study group was more often complicated by PROM in 2 of 31 patients (6.0% ) in GBBS/study group compared to the control group( 0%)(p<0.01) and by preterm labor and delivery in 8 of 31 patients (25.8%)compared to 3 of 31 patients( 9.6%), p<0.01 in the control group. A trend for the PROM existed (6.0% vs 0%) was noted, but not statistically significant, (p=0.1). The incidence of PTL with term delivery and the incidence of associated sexually transmitted diseases (STD) were not significantly different (Table 2).
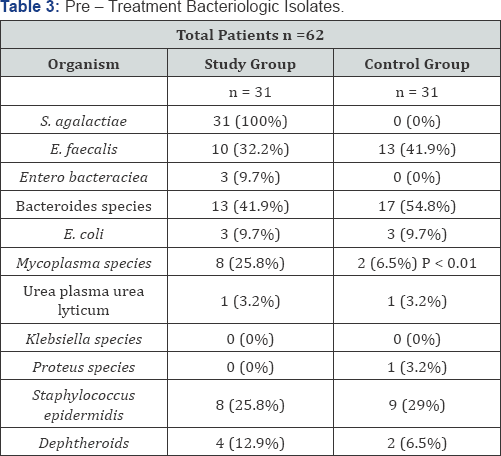
Organisms found in the endometrium prior to antibiotic treatment are shown in Table 3. The most common organisms isolated prior to treatment except GBBS in the study group were Bacteroides, Mycoplasma and Staphylococcus species. The single organism most commonly isolated after treatment was Enterococcus faecalis in 26 of 62 patients (37.1%). Of the 31 patients in the study group with GBBS found in endometrial cultures prior to antibiotic therapy, 14 (45.2%) were noted to have persistence of GBBS in cultures of the endometrium following treatment. There was no significant difference in the rate of cure when evaluated for antibiotic regimen or persistence of GBBS. There was no difference in the other bacteria isolated between the GBBS and control group except for a significant increase in the recovery of the Mycoplasma species in the GBBS study group (25.8% vs 6.5%), p<0.01.
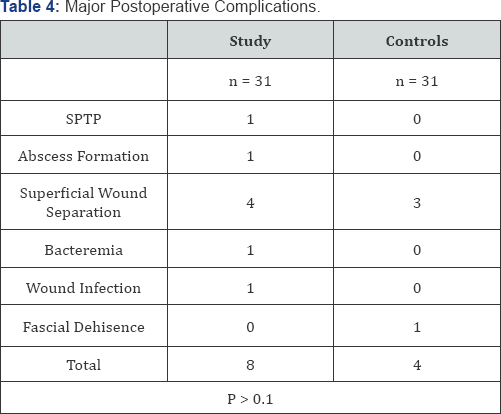
There was a non-significant trend for major post-operative complications including septic pelvic thrombophlebitis, wound separation, fascial dehiscence, wound infection and abscess formation in those patients with GBBS endomyometritis study group than the control grou p(25.8% vs 12.9%), respectively, (p = 0.12) (Table 4). However when specifically looking at infectious complications (abscess, bacteremia, wound infection) there was a statistically significant association in the GBBS study group. Of the 8 patients with major complications in the GBBS group, 5 had persistent Group B streptococcus in repeat endometrial cultures despite treatment with antibiotic regimens demonstrating favorable susceptibility patterns.
Thirteen patients were excluded from evaluation of the persistence of GBBS found in early antenatal period (six from study group and seven from control group) because prenatal cultures for GBBS were not collected.
Four of the 25 (16%) endometritis patients with GBBS at time of diagnosis were found to have cervical colonization at 3233 weeks (three patients) and 14 weeks (one patient). Follow- up cultures of the four patients with the antepartum GBBS were negative in 2 patients; the remaining 2 patients delivered prematurely prior to scheduled follow-up cultures. Of the 24 control group patients with endomyometritis with antenatal screening, only one was positive (at 9 weeks of gestation). A follow-up culture was performed and was negative after treatment. One patient in the study group and two patients in the control group had antenatal urinary tract infections with GBBS. Two of eight patients (25%) with persistent GBBS recovery despite adequate antibiotic treatment, went to the delivery prematurely, compared to 3 of 31(9.7%) patients without GBBS isolates in the early antepartum period.
Discussion
Maternal colonization of the upper genital tract has been demonstrated to have a significant impact on neonatal health, and appears that it may have an adverse effect on maternal health as well. Prenatal screening currently centers on identifying colonized mothers in an attempt to reduce neonatal morbidity and mortality. However, it appears that significant maternal morbidity may exist in mother positive for GBBS in the antepartum period, and even worse if it persists following treatment.
It is apparent that screening and successful antepartum/ intrapartum treatment does not eliminate postpartum GBBS or the maternal complications. This is consistent with M A Krohn and colleagues finding of an increase in intra amniotic and postpartum endometrial infections [8]. Therefore, it appears that identification of patients with persistent GBBS despite treatment may identify those at risk for preterm delivery or sever postoperative infectious complications. One cannot determine from these data if this screening and treatment strategy resulted in a reduction of the overall incidence of GBBS endomyometritis. The success rate of treating endometritis did not differ according to the presence or absence of GBBS, thus antepartum screening should not have an impact on antibiotic choices for treatment of post-partum endometritis.
However as patients with GBBS associated endomyometritis do appear to have a higher serious infectious complication rate, especially if persistent infection was present, it may be prudent to more closely monitor those patients for serious postpartum complications regardless of their treatment regimen. It may be reasonable to obtain endometrial cultures at time of diagnosis of endomyometritis in all patients and if positive for GBBS, reculture endometrium at the end of therapy. In those patients with persistent GBBS, it may be helpful to monitor them more closely for the serious complications prior to and following discharge.
It is uncertain if the initial presence of GBBS is associated with a greater incidence of severe post-operative infectious complications, the persistence of GBBS is significantly associated with these complications.
More research will need to be done to evaluate this strategy and refine the methods. However, in this era of "never-events” and penalties for re-admission, culturing for endometrial GBBS when diagnosed with a postpartum infection may help the physician to identify patients at risk for immediate and delayed serious adverse outcomes.
For more open access journals in JuniperPublishers please click on: https://juniperpublishers.com/
For more articles on Gynecology and Women’s Health please click on: https://juniperpublishers.com/jgwh/
To read more......Fulltext in Gynecology and Women’s Health in Juniper Publishers
https://juniperpublishers.business.site/




Comments
Post a Comment